0:00:10.291,0:00:13.000
Hello and welcome.
0:00:13.791,0:00:15.500
I hope all of you are well.
0:00:15.500,0:00:18.041
My name is Garvia Bailey,
0:00:18.500,0:00:21.875
and I will be your moderator
for today’s symposium.
0:00:22.250,0:00:25.625
Welcome on behalf of the MacKinnon Trauma
and Recovery
0:00:25.625,0:00:29.041
Lab Back Project Health Care Salute.
0:00:29.500,0:00:32.125
This is symposium
number two Risk and Resilience
0:00:32.125,0:00:36.333
in health care providers during the COVID
19 pandemic.
0:00:36.875,0:00:39.083
Now, before I go much further,
it would be rude of me
0:00:39.083,0:00:40.875
not to share a little of myself with you.
0:00:40.875,0:00:43.958
I am a journalist by trade,
a storyteller by nature.
0:00:44.375,0:00:46.833
I’m honored to be with you today.
0:00:46.833,0:00:50.166
My own
family came here from Jamaica in the 1970s
0:00:50.166,0:00:53.166
and we continue to be ever so fortunate
and grateful
0:00:53.583,0:00:57.875
to have come to this country on this land
and on this terror territory.
0:00:58.125,0:01:00.541
As immigrants and settlers.
0:01:00.541,0:01:03.916
I live and work on land that we recognize
as the traditional territories
0:01:03.916,0:01:07.958
at the Haudenosaunee
and Anishinaabe nations and recognize
0:01:07.958,0:01:10.333
and act on the responsibility
that comes with that.
0:01:10.791,0:01:15.333
I’d also like to acknowledge the land
on which McMaster University is located,
0:01:15.541,0:01:20.166
which is also the traditional territory
of the heart, nation and honest
0:01:20.166,0:01:25.000
Nabi nations and within the lands
protected by the dish with one spoon.
0:01:25.000,0:01:28.125
Wampum belt that wampum uses
0:01:28.125,0:01:29.583
the symbolism of a dish
0:01:29.583,0:01:35.083
to represent the territory and one spoon
to represent that the people are to share
0:01:35.083,0:01:39.333
the resources of the land and only take
what they need further to that.
0:01:39.541,0:01:45.375
The Truth and Reconciliation Commission
94 calls to actions and reaffirms
0:01:45.375,0:01:49.041
that the Treaty with Indigenous peoples
must be lawfully honored.
0:01:49.416,0:01:50.541
We are all treaty
0:01:50.541,0:01:54.458
peoples and are responsible for honoring
and upholding those agreements.
0:01:55.500,0:01:59.166
Again, I welcome you to this symposium.
0:01:59.583,0:02:04.291
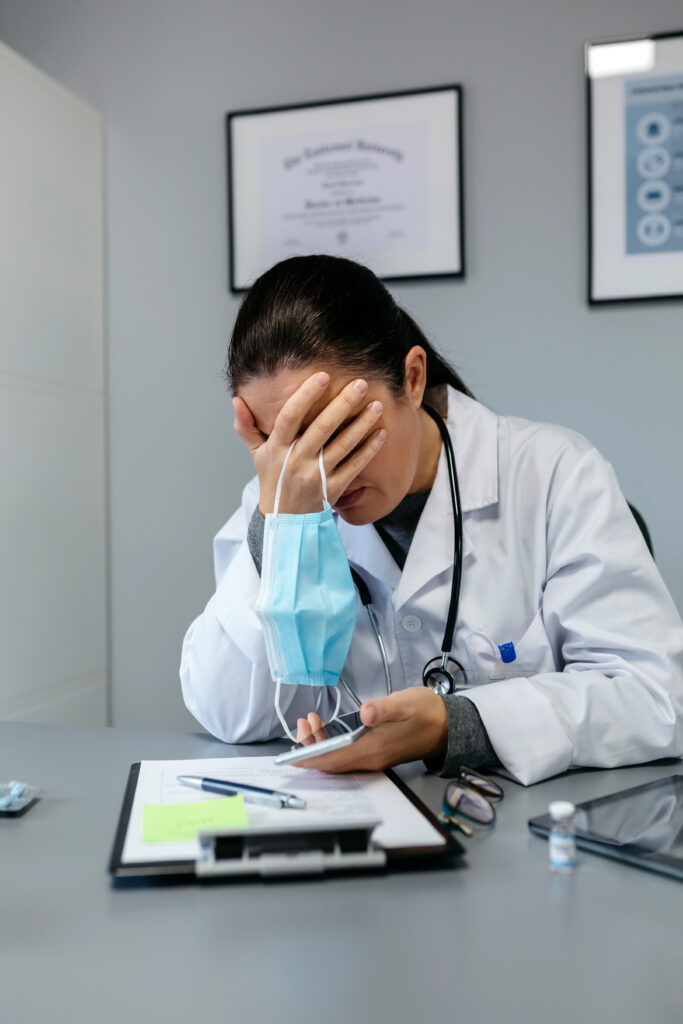
Over the past close to three years,
we’ve heard much about the strain
0:02:04.291,0:02:08.166
of the health care system and on health
care providers due to the pandemic.
0:02:08.458,0:02:10.166
This research project seeks to shine
0:02:10.166,0:02:14.125
a light on the impact that the pandemic
has had on mental health.
0:02:14.125,0:02:17.333
Of all those health care providers
who have given
0:02:17.333,0:02:19.958
and continue
to give so much of themselves.
0:02:20.708,0:02:23.333
So some of you here today
0:02:23.333,0:02:27.041
will hear it will be
it will be a difficult process.
0:02:27.041,0:02:29.750
We’re going to hear a lot of stories.
0:02:29.750,0:02:34.000
We will be discussing instances
of moral distress and moral injury
0:02:34.250,0:02:39.750
and the challenges at home and at work
that health care providers have faced
0:02:40.083,0:02:44.083
and continue to face
during the COVID 19 pandemic.
0:02:44.583,0:02:46.250
We’ll be here together for a while.
0:02:46.250,0:02:48.666
So take the time you need.
0:02:49.083,0:02:52.333
If you need to break, please do so.
0:02:52.333,0:02:53.541
Step out.
0:02:53.541,0:02:54.666
Breathe deeply.
0:02:54.666,0:02:58.708
Do whatever it is necessary
to take good care of yourselves.
0:02:58.958,0:03:03.750
We also have links in the charts
that link to wellness support.
0:03:04.833,0:03:05.583
Take a look.
0:03:05.583,0:03:10.625
And if you need anything, please
do take advantage of those resources.
0:03:11.166,0:03:13.625
Please note that there is closed
captioning
0:03:13.625,0:03:16.500
and transcription and French translation
0:03:16.833,0:03:20.916
available for this event For those
who would like to access those services.
0:03:21.166,0:03:25.375
You’ll see interpretation
on the bottom of the zoom screen
0:03:25.375,0:03:28.958
and you can just hit that and
you can have this in French or English.
0:03:30.416,0:03:32.125
A huge thank you
0:03:32.125,0:03:35.041
to the public Health Agency of Canada
0:03:35.416,0:03:39.458
and all of our partners
for their commitment and support.
0:03:39.708,0:03:44.791
This symposium is being recorded
as part of a broader research project,
0:03:44.791,0:03:46.541
so you’ll have the opportunity
0:03:46.541,0:03:49.833
to revisit the information
that you’ll take in today.
0:03:50.250,0:03:53.541
There is an open chat function
for this virtual event.
0:03:53.583,0:03:57.583
Please be respectful in your interactions
0:03:57.958,0:04:00.583
and try and keep the chat on topic
0:04:01.750,0:04:03.041
and it would be great right now
0:04:03.041,0:04:06.708
if you’re here to get a sense
of where you are logging in from.
0:04:07.166,0:04:10.166
I’m sorry that I don’t have any prizes
for someone that’s coming from far away,
0:04:10.166,0:04:13.625
but we should test this chat
function really quickly.
0:04:13.875,0:04:16.291
Where are you coming from?
0:04:16.291,0:04:19.000
Remember that each section
0:04:19.000,0:04:22.041
today will also be.
0:04:22.041,0:04:23.583
Oh, Innisfil St Thomas.
0:04:23.583,0:04:24.875
Hello, Winnipeg.
0:04:24.875,0:04:27.333
Hello. Good to see you.
0:04:27.333,0:04:30.750
Each section
today will be open to audience questions.
0:04:30.750,0:04:34.750
You can use the Q&A box
to drop in your questions.
0:04:34.750,0:04:39.125
Again, at the bottom of your zoom screen
you will see the Q&A box.
0:04:39.666,0:04:43.583
Now, we won’t be able to get to all of
your questions, but we will do our best.
0:04:44.333,0:04:48.750
Now, links to the extended bios of all
participants can be found on the screen.
0:04:49.125,0:04:50.708
It’s as important.
0:04:52.208,0:04:55.375
So if you’re hearing someone speak
and you want to learn more about them,
0:04:55.583,0:04:58.916
you’ll see that the sessions will be in
0:04:58.916,0:05:01.208
three parts, 1215 will take a break.
0:05:01.958,0:05:08.208
And that, my friends, is the
how of all of this happening today.
0:05:08.250,0:05:11.250
Now I want to tell you
why this research is
0:05:11.250,0:05:15.916
a crucial part of establishing
the spirit of today’s session.
0:05:15.916,0:05:18.958
And with that, I’d like to introduce
and welcome Dr.
0:05:18.958,0:05:22.958
Margaret MacKinnon,
who leads the team on this project.
0:05:23.291,0:05:25.208
Hello, Margaret.
0:05:25.208,0:05:27.333
Garvia, lovely to see you.
0:05:27.333,0:05:29.375
It’s wonderful to see you as well.
0:05:29.791,0:05:34.500
Now, can you tell me first
what you and your colleagues were hearing,
0:05:34.500,0:05:38.875
seeing, experiencing
that kind of set the table for conducting,
0:05:38.875,0:05:42.083
collating this research
that will go through today?
0:05:42.541,0:05:43.916
Thank you so much, Garvia.
0:05:43.916,0:05:47.458
And I want to begin first by thanking
0:05:47.750,0:05:50.625
those of you
who are here today for your service.
0:05:51.250,0:05:54.625
I’ve worked for a very long time
with the military, with veterans
0:05:54.625,0:05:59.125
and first responders, and we often say
we salute you for your service.
0:05:59.500,0:06:04.083
Today, we would like to salute health
care workers across the country,
0:06:04.083,0:06:08.291
in North America and beyond
for their service during the pandemic.
0:06:08.708,0:06:10.750
In many instances,
it is felt like with that war
0:06:10.750,0:06:15.833
footing over the past three years,
and as a clinical psychologist,
0:06:15.833,0:06:20.750
I have the privilege of being on
some of the COVID 19 and ICU units
0:06:20.750,0:06:25.125
to provide mental health supports
to health care workers during the pandemic
0:06:25.500,0:06:29.458
and to hear their stories,
to learn of the sacrifices that they
0:06:29.458,0:06:33.125
and their family members were making,
and to see the distress
0:06:33.416,0:06:37.291
that many of them were in over
the course of the pandemic
0:06:37.583,0:06:41.958
as it now continues
and into the aftermath, we hope, one day.
0:06:42.291,0:06:45.875
We just want to be there to support
health care workers, to hear
0:06:45.875,0:06:50.625
and know their stories,
and also to thank them for their service.
0:06:51.125,0:06:52.541
Mm hmm.
0:06:52.541,0:06:57.041
Now, Margaret, why are risk and resiliency
0:06:57.041,0:07:01.250
in tandem for our discussion today
so much Garvia.
0:07:01.291,0:07:06.166
You know, all of us have individual
reactions to what’s happening right now.
0:07:06.166,0:07:09.541
And for some people,
there will be things that contribute
0:07:09.541,0:07:12.666
to resiliency,
to making things a bit easier
0:07:13.000,0:07:16.083
to to cope with, with what health care
workers are facing.
0:07:16.416,0:07:18.666
There are also factors
that contribute to risk.
0:07:18.666,0:07:22.083
And we know, for example,
having experienced childhood abuse
0:07:22.083,0:07:25.291
and neglect, for example,
can make one more vulnerable
0:07:25.541,0:07:30.375
to experiencing strong emotions
from the situations that people face.
0:07:30.666,0:07:35.541
We know that not having a support system
or not having access to a support system
0:07:35.541,0:07:40.041
is also very much a risk factor
for experiencing mental health
0:07:40.041,0:07:43.375
difficulties and during the pandemic,
what we heard from many health
0:07:43.375,0:07:46.208
care workers, we’ve interviewed over
124 health care workers
0:07:46.541,0:07:49.291
across the country
and survey close to 600 now.
0:07:49.666,0:07:52.541
And what we hear
is that, you know, during the pandemic,
0:07:52.541,0:07:56.791
there were access to gyms
being able to see friends and family.
0:07:57.000,0:07:58.625
These were things
that often weren’t available.
0:07:58.625,0:08:01.791
And so we want to look at what
are some of the factors that help people
0:08:02.041,0:08:04.875
on their mental health journey
and what are some of the factors
0:08:04.875,0:08:08.416
that contribute to risk
if we know what those risks are?
0:08:08.708,0:08:11.750
And we’re going to hear that today from
the work that we’re going to hear about.
0:08:12.041,0:08:15.333
And we can target these areas
to try to prevent
0:08:16.000,0:08:20.666
or at least to help heal
some of the mental health workers there.
0:08:20.708,0:08:26.583
So, for example, can we set up social
support systems for via the Internet
0:08:26.583,0:08:30.166
or other means where we can support health
care workers and what they’re facing?
0:08:30.500,0:08:34.125
You know, being on the units, what I saw
so often with the strength of team
0:08:34.416,0:08:38.083
and the strength of together nurse
and health care workers often talked about
0:08:38.083,0:08:39.166
how they didn’t
0:08:39.166,0:08:42.000
want to go home because they felt
they were letting their team down.
0:08:42.333,0:08:43.500
We want to find that space
0:08:43.500,0:08:47.166
for self-compassion
and putting the oxygen mask on ourselves
0:08:47.500,0:08:51.208
so that we can help others and also
strengthening and building our teams.
0:08:52.125,0:08:53.791
Mm hmm. Absolutely.
0:08:55.333,0:08:55.916
You know, we’re going to
0:08:55.916,0:08:58.750
have a very deep conversations.
0:08:59.166,0:09:01.125
We’re going to hear a lot of stories.
0:09:01.125,0:09:05.750
And I wonder about where you’d like
this conversation to go next.
0:09:06.125,0:09:10.500
Once we’ve, you know, all the researchers
we’ve had, all the this
0:09:10.958,0:09:13.416
this what I will probably,
0:09:14.500,0:09:17.333
I think is going to be like
a real groundswell
0:09:17.333,0:09:19.375
of of support for this project.
0:09:19.625,0:09:21.541
What happens next?
0:09:21.625,0:09:21.916
Yeah.
0:09:21.916,0:09:24.541
And, you know, I’m going to think
about where I was last night.
0:09:24.541,0:09:26.916
So I was speaking to the Saskatchewan
union nurses.
0:09:26.916,0:09:30.833
And you know what we’ve heard in these
interviews from health care workers,
0:09:30.875,0:09:34.750
The first thing that they ask
for people to know their stories,
0:09:34.750,0:09:37.750
they don’t want to have to tell
the stories over and over again.
0:09:38.125,0:09:42.000
Many people feel alone in the struggles
that they face.
0:09:42.416,0:09:45.541
I mean, they want policymakers,
they want clinicians.
0:09:45.875,0:09:49.583
They want members of the public
to know what their struggles have been.
0:09:50.166,0:09:53.583
And we think about how we support health
care workers as both thanking them,
0:09:53.583,0:09:57.041
knowing their stories
and setting up systems and supports
0:09:57.333,0:09:59.791
that will be available
to these healthcare workers.
0:10:00.208,0:10:02.166
A lot of the work that we’re doing
for the Public Health Health
0:10:02.166,0:10:05.958
Agency of Canada and other groups across
the country are doing is really to set up
0:10:06.083,0:10:09.041
concrete supports
that are available to health care workers
0:10:09.500,0:10:12.666
and also first responders and public
safety personnel who have served
0:10:12.791,0:10:15.958
in other essential workers
who have suffered because of the pandemic.
0:10:16.375,0:10:19.208
I think at the federal level,
we really want to talk about
0:10:19.208,0:10:23.333
organized supports that are equitable
and available to all Canadians.
0:10:23.958,0:10:25.291
So we think about individuals,
for example,
0:10:25.291,0:10:27.708
who are joining us
from the Northwest Territories today.
0:10:28.208,0:10:33.166
How do we ensure that the supports that we
provide are available to all Canadians,
0:10:33.166,0:10:35.708
those who serve,
and also the general population
0:10:35.708,0:10:38.041
who have really experienced
a lot of mental health
0:10:38.041,0:10:39.541
difficulty throughout this as well.
0:10:39.541,0:10:43.625
But we place here a very special emphasis,
a very special thank you
0:10:44.041,0:10:47.583
to those who have served a great sacrifice
not only to themselves,
0:10:47.916,0:10:49.708
but also to their families.
0:10:49.708,0:10:53.041
And we’ve heard from nurses,
physiotherapists, occupational therapists
0:10:53.041,0:10:57.666
say, when I get home,
I have two words maybe left for my family.
0:10:57.875,0:10:59.791
I’m so tired.
0:10:59.791,0:11:02.166
We know that the partners
0:11:02.166,0:11:05.041
parents have taken over
caregiving responsibilities.
0:11:05.458,0:11:09.500
So collectively
there has been a great deal of service
0:11:09.500,0:11:13.625
and sacrifice and we need to be available
and have mechanisms
0:11:13.625,0:11:16.500
to support those individuals
and their families.
0:11:17.375,0:11:19.000
Yeah, absolutely.
0:11:19.000,0:11:20.375
Well, thank you so much.
0:11:20.375,0:11:24.041
We’re going to dive in right now.
0:11:24.541,0:11:26.125
Thank you, Margaret.
0:11:26.125,0:11:28.958
Now I’m going to turn it over to Dr.
0:11:28.958,0:11:34.125
Kim Ritchie and Mina Pichtikova
with a summary of the research
0:11:34.125,0:11:37.041
findings on moral injury
in Canadian health care
0:11:37.333,0:11:46.125
providers.
0:11:50.500,0:11:51.125
Hi, everyone.
0:11:51.125,0:11:53.041
My name is Mina Pichtikova to cover,
0:11:53.041,0:11:56.916
and today I’ll be presenting alongside
my wonderful colleague, Dr.
0:11:56.916,0:12:01.416
Kimberly Ritchie on the topic
of resilience among health care workers.
0:12:02.583,0:12:04.958
So before we get started,
it’s important to highlight
0:12:04.958,0:12:07.916
what resilience is
and why it’s so important.
0:12:08.458,0:12:11.208
So there are a lot of different
definitions of resilience,
0:12:11.208,0:12:13.208
but the most straightforward one
0:12:13.208,0:12:16.041
and the one that we’ve used
for the purpose of this study
0:12:16.416,0:12:20.583
is that resilience is the ability
to bounce back or recover from stress.
0:12:21.541,0:12:24.125
And what resilience really allows
one to do
0:12:24.125,0:12:27.375
is to cope with adversities
that occur during stressful periods,
0:12:27.666,0:12:31.291
which may otherwise trigger mental
or psychological problems.
0:12:32.083,0:12:35.041
And to highlight that point,
there is ample evidence to suggest
0:12:35.041,0:12:38.125
that during stressful events
such as disasters
0:12:38.125,0:12:41.250
or disease outbreaks,
in the case of the COVID 19 pandemic,
0:12:42.333,0:12:43.416
people are more likely to
0:12:43.416,0:12:46.750
suffer negative mental
health and psychologic consequences
0:12:47.250,0:12:50.083
when they’re not equipped with ample
0:12:50.083,0:12:53.375
levels of resilience.
0:12:53.500,0:12:56.208
Now, this is especially true
for health care providers
0:12:56.708,0:13:00.708
in recent years during the pandemic,
as they’ve repeatedly been faced
0:13:00.708,0:13:05.291
with increasingly stressful situations
for a very prolonged period of time now.
0:13:06.166,0:13:09.583
And now what we’re seeing
is that as a result, health
0:13:09.583,0:13:12.250
care providers have suffered
an immense deterioration
0:13:12.250,0:13:15.041
in their mental and psychological health
during the pandemic
0:13:15.541,0:13:18.500
on a number of different measures,
including anxiety,
0:13:18.791,0:13:23.041
depression, burnout,
PTSD and psychological distress.
0:13:23.041,0:13:25.625
And they’re experiencing
0:13:25.625,0:13:27.541
these this deterioration in mental health
0:13:27.541,0:13:29.916
at higher levels than the general public.
0:13:30.875,0:13:34.083
So that being said, resilience
isn’t something that’s set in stone
0:13:34.375,0:13:37.958
and it can be influenced either positively
or negatively
0:13:38.250,0:13:41.750
by a number of different factors,
including individual factors,
0:13:42.041,0:13:45.208
organizational factors,
or even societal factors.
0:13:46.083,0:13:48.291
So all those things considered resilience
0:13:48.291,0:13:51.333
is an incredibly important concept
for us to explore.
0:13:52.000,0:13:55.250
And what we’ll be talking about
today is our study
0:13:55.250,0:13:58.583
on the relationship between resilience
and a number of different variables,
0:13:59.041,0:14:00.791
including mental health,
0:14:00.791,0:14:05.458
burnout, organizational support
and social support, just to name a few.
0:14:06.458,0:14:07.833
And ultimately, doing
0:14:07.833,0:14:11.750
this is incredibly important,
as it seems that resilience is likely
0:14:11.750,0:14:15.416
a strong safeguard of mental health
among health care providers.
0:14:15.750,0:14:16.458
And exploring
0:14:16.458,0:14:20.375
these questions will ultimately allow us
to develop and implement interventions
0:14:20.750,0:14:25.583
that are aimed towards using evidence
based interventions to enhance resilience
0:14:25.583,0:14:30.250
and strengthen health care providers
defenses against the various mental
0:14:30.250,0:14:33.125
health and psychological consequences
of the pandemic.
0:14:33.833,0:14:36.666
So just to give you
a little bit of a brief overview of
0:14:37.041,0:14:38.416
how our study was set up.
0:14:38.416,0:14:41.833
So we started off with the recruitment
stage where we invited
0:14:42.125,0:14:45.333
Canadian Health care workers
who were directly or indirectly involved
0:14:45.666,0:14:50.375
in patient care during the COVID 19
pandemic to participate in.
0:14:50.375,0:14:55.958
The first thing they did was fill out
a collection of online questionnaires.
0:14:56.416,0:15:00.041
So a total of 460 health care providers
0:15:00.958,0:15:05.708
filled out the questionnaires
May 20, 22 to January 2023.
0:15:06.166,0:15:09.083
And then some of those participants
were also that indicated
0:15:09.083,0:15:13.083
they were interested in being interviewed,
were invited to a virtual interview,
0:15:13.333,0:15:14.708
and the interview was semi-structured.
0:15:14.708,0:15:17.875
That was kind of to get more
into the nuances of their experiences.
0:15:18.458,0:15:23.458
And then a quantitative and qualitative
analysis was done on the
0:15:24.166,0:15:27.375
questionnaire data and the interview
transcripts, respectively.
0:15:28.500,0:15:29.083
So in terms
0:15:29.083,0:15:33.666
of the demographics of the individuals
who participated in the study,
0:15:34.333,0:15:36.750
the average age was 43 years old,
0:15:37.416,0:15:40.500
and about 50% of our participants
were nurses.
0:15:40.916,0:15:43.625
The majority of them came
from the province of Ontario.
0:15:43.625,0:15:49.041
Specifically, it’s 64%
and 89% of them identified as female.
0:15:49.750,0:15:53.166
So another questionnaire
that we used to capture resilience,
0:15:53.916,0:15:56.166
this is the brief resilience scale.
0:15:56.166,0:15:59.166
And essentially like we discussed earlier,
it assesses
0:15:59.166,0:16:01.541
one’s ability to bounce back
or recover from stress.
0:16:02.166,0:16:04.750
And I’ve put items up here
just so you can kind of get a sense
0:16:04.750,0:16:06.791
of the kinds of questions
people were asked.
0:16:06.791,0:16:10.083
And the brief resilience scale
is an established, reliable
0:16:10.083,0:16:12.666
and valid measure of assessing resilience.
0:16:13.375,0:16:15.791
So now that we know why resilience
0:16:15.791,0:16:20.041
is so important, let’s explore what our
what story does
0:16:20.041,0:16:23.583
our data tell us and unfortunately, it’s
not a very good one.
0:16:23.583,0:16:29.541
So out of the 460 participants,
51% scored in the range of low
0:16:29.541,0:16:34.583
resilience, 45%
scored in the normal resilience range
0:16:35.000,0:16:39.500
and only 3.5%
scored in the high resilience range.
0:16:40.416,0:16:44.250
So what we did next was a correlation
analysis, which is essentially
0:16:44.250,0:16:48.958
just a statistical test
to explore how variables are related.
0:16:49.625,0:16:53.416
Specifically, we were interested in
how resilience is related
0:16:53.416,0:16:57.541
to all the variables that I’ve listed here
in blue on the right.
0:16:58.166,0:17:01.291
And all of this was done
using the questionnaire data.
0:17:01.291,0:17:05.333
And what we see by this is that resilience
is significantly negatively
0:17:05.333,0:17:08.125
correlated
with all these variables in blue,
0:17:08.833,0:17:11.916
which means that people
who reported higher levels of resilience
0:17:12.333,0:17:17.000
reported experiencing less moral injury,
PTSD,
0:17:17.541,0:17:21.166
burnout, insomnia, depression,
0:17:21.166,0:17:25.083
anxiety,
stress and emotional dysregulation.
0:17:26.041,0:17:28.791
Now, PTSD in moral
injury is something that we’re hearing
0:17:28.791,0:17:31.916
about a lot lately
amongst health care providers,
0:17:32.375,0:17:36.958
and so we thought it would be worth it
to explore these two variables further.
0:17:37.625,0:17:41.833
So along the horizontal, horizontal axis,
we have resilience,
0:17:41.958,0:17:44.750
specifically
low normal and high resilience,
0:17:45.916,0:17:49.208
and we see very similar
trends amongst the two graphs.
0:17:49.875,0:17:52.416
So on the graph on the left,
we’re looking at
0:17:52.416,0:17:56.250
how resilience is associated
with PTSD symptoms,
0:17:56.583,0:18:01.208
which were assessed
using the PCL five questionnaire.
0:18:02.541,0:18:06.333
And what we see is that individuals
who have low resilience
0:18:07.458,0:18:09.958
have significantly higher levels of PTSD
0:18:09.958,0:18:12.041
symptoms than those with high resilience.
0:18:13.250,0:18:17.291
And then the same trend is seen
on the graph on the right, which explores
0:18:17.291,0:18:21.625
moral injury, and that was measured
using the moral injury outcome scale.
0:18:21.916,0:18:25.166
So once again, we see that individuals
who have low resilience
0:18:25.625,0:18:26.875
experienced significantly
0:18:26.875,0:18:30.375
higher levels of moral injury
than those with high resilience.
0:18:31.041,0:18:33.458
We also looked
at a number of questionnaires related
0:18:33.458,0:18:37.458
to organizational, social
and self-compassion factors.
0:18:38.041,0:18:40.958
And what we see here
is that resilience is significantly,
0:18:40.958,0:18:43.625
positively correlated
with all these variables.
0:18:44.250,0:18:46.500
So what that means is that
0:18:46.833,0:18:51.875
people who reported higher levels
of resilience reported experiencing
0:18:52.000,0:18:55.875
more organizational support,
more self-compassion,
0:18:56.416,0:19:00.333
more social support
and more product unity in their workplace.
0:19:01.291,0:19:03.666
Interestingly, resilience
was also associated
0:19:03.666,0:19:07.000
with the years
someone has worked and their age,
0:19:07.500,0:19:10.416
such that individuals
who had worked in the field longer
0:19:10.458,0:19:13.916
or were older reported
higher levels of resilience.
0:19:14.500,0:19:17.666
So now I’ve just put up the actual names
0:19:17.666,0:19:22.083
of the questionnaires that we use
to capture these different factors.
0:19:22.333,0:19:23.791
In case anyone is interested.
0:19:24.958,0:19:27.458
And now I’m going to pass it off
to my colleague, Dr.
0:19:27.458,0:19:28.750
Kim Ritchie, who’s going to explore
0:19:28.750,0:19:31.291
the qualitative bit of this study
a bit more with you.
0:19:32.958,0:19:34.416
Thank you, Mina.
0:19:34.416,0:19:38.708
And as Mina mentioned, my name is Kim
Richey, and today I’m going to present
0:19:38.708,0:19:42.750
some of our preliminary findings
from the qualitative part of our research.
0:19:43.208,0:19:48.333
And in this part, we took a deeper look
at some of the work and personal factors.
0:19:48.333,0:19:52.416
Associate with resiliency of health
care providers during the pandemic.
0:19:53.250,0:19:56.541
For this part of our study,
we included health care providers
0:19:56.833,0:19:58.291
who completed an interview.
0:19:58.291,0:20:02.000
In addition to the survey,
and we included those participants
0:20:02.000,0:20:05.541
who scored either in the lower
or the higher ranges
0:20:05.541,0:20:09.583
on the brief resilience scale,
which was part of the online survey.
0:20:10.291,0:20:13.500
We then analyzed their interview data
in two groups
0:20:13.958,0:20:17.958
the health care providers who had lower
scores on the brief resilience scale
0:20:18.333,0:20:21.375
and those who scored in the higher score
higher range.
0:20:21.375,0:20:23.375
On the brief Resilience scale.
0:20:23.375,0:20:27.541
This analysis included
23 participants in total
0:20:28.041,0:20:31.916
and they represented
several different health care occupations,
0:20:31.916,0:20:36.750
including nursing, occupational therapy,
respiratory therapy and so on.
0:20:37.625,0:20:41.250
In our analysis,
we found three themes that cross-cut
0:20:41.583,0:20:44.625
the lower
and higher resiliency group today.
0:20:44.625,0:20:45.125
All share
0:20:45.125,0:20:49.416
those three themes, along with a quote
from each group to describe that theme.
0:20:49.958,0:20:53.958
In the first theme, participants in
both groups described many similarities
0:20:53.958,0:20:57.416
in the type of coping strategies, say,
utilized during the pandemic.
0:20:58.000,0:21:01.208
Overall, many participants reported
the pandemic
0:21:01.208,0:21:05.583
had a drastic impact on their ability
to practice usual coping strategies
0:21:06.000,0:21:10.166
with the loss of going to the gym
or visiting friends and family
0:21:10.166,0:21:14.916
and so on, due to especially during
the during the periods of lockdown.
0:21:15.541,0:21:20.333
And because of that, they really had
to adapt and develop new ways of coping.
0:21:21.041,0:21:24.333
The most common coping strategies found in
both groups
0:21:24.708,0:21:28.916
was an increase
in their use of alcohol, use of marijuana.
0:21:28.916,0:21:34.000
Sometimes for the first time,
eating more increased use of social media,
0:21:34.333,0:21:38.791
going for long walks
and increased risk taking behavior.
0:21:38.791,0:21:41.041
And these were all ways to manage
0:21:41.041,0:21:44.416
the increased stress they were
experiencing during the pandemic.
0:21:45.208,0:21:47.916
So, for example, the quotes on this slide
0:21:48.291,0:21:52.625
four in both the higher and Lower
Resilience Group report, similar
0:21:52.625,0:21:56.625
use of increase are similar increased
use of alcohol
0:21:56.916,0:21:59.916
as a way to help them cope
with their stress after work.
0:22:00.875,0:22:01.333
Several
0:22:01.333,0:22:04.250
participants also reported
that they recognized
0:22:04.666,0:22:08.208
that they were struggling
and they had a lot of increased stress.
0:22:08.958,0:22:13.875
They were to the point of exhaustion
and they came to realize that they had
0:22:13.875,0:22:17.041
to really prioritize their own self-care
0:22:17.458,0:22:20.083
over their need to care for others.
0:22:20.583,0:22:23.625
And we heard also about this
from health care
0:22:23.625,0:22:27.000
providers in both the lower
and higher resilience groups.
0:22:27.000,0:22:32.208
And they also they talked about having
this real difficulty or even a tension
0:22:32.541,0:22:37.208
when it came to prioritizing their health
and well-being over others.
0:22:37.625,0:22:40.833
And the reason for this
was that health care providers
0:22:41.083,0:22:44.375
really see themselves
as individuals who care for others.
0:22:44.791,0:22:47.458
And it is a big part of their identity.
0:22:47.916,0:22:52.750
Therefore, it’s really hard for them
to turn that same care towards themselves
0:22:52.958,0:22:57.583
or even to balance care for themselves
with their care for others.
0:22:58.875,0:23:01.416
Some of the health care providers
we talked to reported
0:23:01.416,0:23:05.416
that they had to give themselves
permission to care for themselves.
0:23:05.416,0:23:09.875
And this was the word that they used over
and over again in the data.
0:23:10.833,0:23:15.208
Sometimes some health care
providers said that they were able
0:23:15.208,0:23:18.291
to give themselves permission
to care for themselves
0:23:18.291,0:23:21.041
or to balance caring for themselves
with others.
0:23:21.541,0:23:24.333
And others said that they
they really wanted
0:23:24.333,0:23:27.458
and needed this permission
to come from someone else,
0:23:27.791,0:23:32.041
such as a family member,
a colleague, or even a supervisor.
0:23:32.583,0:23:36.625
And having this permission
given to them really helped them
0:23:36.625,0:23:40.208
to resolve some of this tension or guilt
they were experiencing
0:23:40.583,0:23:45.750
when it came to turning
that care towards themselves.
0:23:45.750,0:23:50.708
And the last thing today
really focuses on the types of ways
0:23:50.708,0:23:54.916
organizations supported
health care providers during the pandemic.
0:23:54.916,0:23:58.000
Most of the health care providers
we spoke with talked
0:23:58.000,0:24:01.625
about long standing challenges
related to being short staffed,
0:24:02.041,0:24:05.583
which was, of course, amplified
during the pandemic and contributed
0:24:05.791,0:24:10.625
to their increased workload and stress
where there were differences in the data.
0:24:10.625,0:24:15.000
So between the two groups within
how their health care providers
0:24:15.000,0:24:19.458
perceive their organizations managed
some of these increased work challenges.
0:24:20.125,0:24:22.458
What we found
was that health care providers
0:24:22.458,0:24:26.541
in the Lower Resilience Group
reported that they didn’t feel supported
0:24:26.916,0:24:31.000
or their organization
wasn’t receptive to their opinions,
0:24:31.958,0:24:34.125
so it didn’t feel safe
0:24:34.125,0:24:38.375
to them or they didn’t have an opportunity
to voice their opinions
0:24:38.875,0:24:41.708
about some of these challenges
that they were experiencing.
0:24:42.291,0:24:46.291
Whereas health care providers
in the Higher Resilience Group talked
0:24:46.291,0:24:52.041
about having a more open environment
in their organization, which was flexible.
0:24:52.416,0:24:56.500
There were established channels
of communication through regular meetings
0:24:56.500,0:25:01.708
or even daily huddles,
and during these times they felt able
0:25:01.708,0:25:05.708
to give their thoughts and opinions
and they felt their voice was heard.
0:25:06.875,0:25:10.083
So in conclusion,
what we found from our research
0:25:10.083,0:25:13.750
was that health care providers
with higher levels of resilience
0:25:13.750,0:25:18.333
may experience less negative mental
health symptoms such as PTSD,
0:25:18.333,0:25:21.541
moral injury, depression,
anxiety and stress.
0:25:22.208,0:25:24.583
Higher resilience is also associated
0:25:24.583,0:25:27.791
with health care providers
who have more social support,
0:25:28.208,0:25:33.875
more self-compassion and perceived,
more supportive organizations.
0:25:33.875,0:25:36.416
Secondly, health care providers
0:25:37.625,0:25:38.833
with both higher and
0:25:38.833,0:25:43.250
lower levels of resilience
have similar types of coping strategies
0:25:43.708,0:25:47.875
and difficulty prioritizing
or balancing their own self-care.
0:25:49.291,0:25:51.750
But there’s differences
in their perception
0:25:51.750,0:25:56.708
of how their organizations were able
to support them during the pandemic.
0:25:57.708,0:26:03.541
Thank you very much.
0:26:03.541,0:26:05.916
Thank you very much.
0:26:05.916,0:26:09.125
That was a fascinating Dr.
0:26:09.125,0:26:12.708
Kim Ritchie and Mina pitch to cover.
0:26:14.375,0:26:17.708
I do have some questions for you,
and I’m sure the audience
0:26:17.708,0:26:21.000
will have questions as well,
those that are listening.
0:26:21.000,0:26:25.500
And just a reminder
that if you’d like to ask
0:26:26.125,0:26:28.208
Mina and Kim any questions,
0:26:28.583,0:26:31.333
you can put your questions in the Q&A
0:26:31.333,0:26:34.916
box as you see that running below there.
0:26:35.250,0:26:37.958
And and I would be happy to to pass
0:26:37.958,0:26:41.375
those questions
on to our panelists for you.
0:26:41.791,0:26:45.833
But for now, Mike, I have some questions
of my own, if that’s okay.
0:26:47.375,0:26:49.000
Now, you
0:26:49.000,0:26:51.875
talked you touched on the personal factors
0:26:52.500,0:26:55.500
that influence resilience.
0:26:55.500,0:27:00.375
And I’m wondering if we can unpack that
just a little bit for for individuals
0:27:01.041,0:27:03.708
when we go back and take this information
and think about
0:27:04.000,0:27:07.875
what are those personal factors
that can be shifted or can be that
0:27:07.875,0:27:12.416
we can think about
in terms of individual resilience?
0:27:12.416,0:27:14.875
What are those personal factors
that influence?
0:27:17.583,0:27:18.291
Hi, Garvia.
0:27:18.291,0:27:23.958
Thank you for having me and for this
opportunity and for the great question.
0:27:24.291,0:27:27.333
So like I mentioned earlier,
the good thing about resilience is that
0:27:27.375,0:27:31.500
it’s not something that’s set in stone
and it’s something that can be influenced
0:27:32.500,0:27:36.000
and something that we can change
at the individual or personal level
0:27:36.291,0:27:39.000
and also at the organizational level.
0:27:39.000,0:27:41.625
In some ways,
to build resilience on a personal
0:27:41.625,0:27:44.708
level is through connection, for instance.
0:27:44.708,0:27:48.583
So building connections
with those that support you because it’s
0:27:48.583,0:27:52.125
very easy to isolate yourself
during hard times,
0:27:52.916,0:27:57.208
but building a sense of community
and being around people that have a common
0:27:57.208,0:28:01.000
understanding can really allow you
to connect with others
0:28:01.000,0:28:02.791
and overcome challenges as a group
0:28:04.250,0:28:06.875
and really allow you to bounce back
from that stress.
0:28:07.750,0:28:10.541
And then another thing
is taking care of your personal wellness.
0:28:11.041,0:28:14.916
So stress is not something
that’s just felt psychologically,
0:28:14.916,0:28:17.833
but it’s also felt in the physical body.
0:28:18.875,0:28:23.291
So of course, self-care is often
easier said than it’s done,
0:28:24.000,0:28:27.416
but it’s important to make it a priority
and give yourself
0:28:27.416,0:28:31.500
that self-compassion
and that space to take care of yourself.
0:28:31.500,0:28:35.541
Like Kim was mentioning earlier.
0:28:35.541,0:28:38.666
Yeah, and take care of the stress,
not only emotionally but physically,
0:28:40.208,0:28:43.083
so that you kind of have
0:28:43.083,0:28:45.625
the ability to push through.
0:28:47.041,0:28:51.750
So this can be like little things
that people build into their wellness
0:28:51.750,0:28:55.958
routines,
getting enough sleep, exercising,
0:28:56.708,0:29:01.041
building healthier habits,
and even small changes can make really
0:29:02.125,0:29:05.333
kind of big effects down the road.
0:29:06.041,0:29:08.000
And another thing is healthy thinking.
0:29:08.000,0:29:11.916
So acknowledging and accepting
your thoughts and emotions during
0:29:11.916,0:29:15.750
stressful times, it’s very natural
for these thoughts and emotions to come up
0:29:17.791,0:29:20.500
and giving
yourself grace when they do come up.
0:29:20.500,0:29:26.416
So kind of reflecting on your thoughts,
are they positive or negative?
0:29:26.416,0:29:28.000
Are they realistic?
0:29:28.000,0:29:30.708
Are they grounded in fact
0:29:30.708,0:29:33.000
and identifying areas of hope
0:29:33.000,0:29:35.666
that you can lean on
0:29:36.666,0:29:38.208
as well as accepting
0:29:38.208,0:29:40.833
certain circumstances
that can’t be changed right now
0:29:41.875,0:29:44.041
and focusing on the things
that you can change?
0:29:44.708,0:29:46.833
And finally
0:29:46.916,0:29:49.291
finding meaning and purpose
in what you’re doing.
0:29:49.291,0:29:55.750
Of course, health care is an incredibly
meaningful and purposeful profession,
0:29:55.750,0:30:02.041
but kind of celebrating your own strengths
and goals and moving towards your values
0:30:02.041,0:30:06.750
or something that can kind of help
foster that resilience.
0:30:06.750,0:30:11.375
But yes, just as much as you know,
there’s these factors
0:30:11.375,0:30:13.958
that are individual
that influence resilience.
0:30:14.541,0:30:17.833
Like I said, there’s also
the organizational and societal factors
0:30:17.833,0:30:19.000
that play a huge role.
0:30:20.625,0:30:23.458
So it’s also important to
0:30:23.458,0:30:26.041
shift away from thinking about this
0:30:26.041,0:30:30.291
as just a personal responsibility
and also thinking about it
0:30:30.291,0:30:35.458
as a societal
and organizational responsibility as well.
0:30:35.458,0:30:37.125
Yeah, absolutely.
0:30:37.125,0:30:40.708
The B it’s interesting
because I feel like the the,
0:30:40.958,0:30:43.916
the personal part of it
0:30:43.916,0:30:47.375
has is a lot like working out
Like it’s a lot
0:30:47.375,0:30:50.750
like the things that you’re supposed to do
for your for your body.
0:30:50.750,0:30:53.958
You think to yourself,
I need to think in this way.
0:30:53.958,0:30:56.708
I need to do these things
and give myself permission
0:30:56.708,0:31:00.708
to feel these feelings
and then and build my resilience. But
0:31:02.083,0:31:04.791
there’s another part of you
that said, I’m just so tired.
0:31:05.083,0:31:09.000
Like, I’m too tired
to think about taking care of myself.
0:31:09.000,0:31:14.750
I’m too tired to think about going to
the gym or, you know, of my own self-care.
0:31:14.750,0:31:16.500
And as your research shows,
0:31:16.500,0:31:20.625
so many people are preoccupied as well
with taking care of others.
0:31:22.416,0:31:25.750
So so I wonder about those small
0:31:27.208,0:31:29.750
the way to perhaps implement
0:31:29.750,0:31:33.958
the smaller parts of building up
the strength, like when you go to the gym,
0:31:33.958,0:31:37.708
you build up the strength
to be able to do the heavier lifting,
0:31:39.208,0:31:42.500
how you want those small bits
0:31:42.500,0:31:46.416
of that personal part
and then the occupational part as well.
0:31:47.041,0:31:51.375
The small things that employers or
those around you communities can be doing.
0:31:52.041,0:31:54.500
Mhm. Yeah, that’s a great point.
0:31:54.500,0:31:56.958
And that’s kind of the catch 22
that we’re seeing
0:31:58.083,0:32:01.750
on one hand,
you know, self care, resilience, wellness,
0:32:02.041,0:32:07.000
it’s incredibly important
and it’s like a muscle that you build up,
0:32:07.708,0:32:12.333
but then when there’s not the space
and the time and people are so burnt out
0:32:12.333,0:32:16.500
that they don’t have the capacity
and it just feels like, yeah, another task
0:32:16.500,0:32:19.625
and yet another responsibility,
that’s kind of when we get trapped
0:32:19.625,0:32:24.250
in that vicious cycle and I think that’s
why it’s so important to highlight
0:32:25.291,0:32:26.375
the organizational
0:32:26.375,0:32:30.708
factors that can influence resilience
and to shift away
0:32:30.708,0:32:34.041
from considering resilience
as just just at the individual level
0:32:34.958,0:32:38.416
that’s fully solvable by people
making life changes.
0:32:38.750,0:32:42.125
But we’re seeing that that’s not the case
0:32:42.125,0:32:44.333
and we’re starting to shift away
from thinking it,
0:32:44.500,0:32:48.291
thinking about it in that way,
and kind of shifting
0:32:48.291,0:32:53.041
some of the responsibility
towards the workplace environment.
0:32:53.041,0:32:56.041
And that includes things
like creating realistic
0:32:57.125,0:32:59.583
and compassionate team culture
0:32:59.916,0:33:02.416
where people can have honest conversations
0:33:03.291,0:33:06.250
with one another.
0:33:06.250,0:33:11.375
You know, organizations
being vigilant about the risks associated
0:33:11.375,0:33:16.208
with the profession and monitoring
ongoing stressors for health care workers,
0:33:17.375,0:33:19.500
having proper staffing,
0:33:19.500,0:33:24.291
having opportunities to discuss
work life balance
0:33:24.291,0:33:30.208
without fear of repercussion,
having having a shared responsibility
0:33:30.541,0:33:35.166
to identify the sources of stress
and take the appropriate measures
0:33:37.333,0:33:39.208
in the workplace.
0:33:39.541,0:33:40.666
Yeah, yeah.
0:33:40.666,0:33:44.208
And I think a lot of this comes down
to also just having
0:33:44.500,0:33:49.291
really clear organizational support
and having policies
0:33:49.291,0:33:52.541
that protect health care providers as well
0:33:54.000,0:33:57.333
so that there isn’t fear of repercussion
0:33:58.291,0:34:02.041
if individuals are bringing up
any sort of organizational concerns.
0:34:03.000,0:34:05.250
So yeah, I think it’s
0:34:05.250,0:34:07.750
definitely a delicate dance
between the two.
0:34:09.166,0:34:12.833
And there are things
at the individual level that, you know,
0:34:13.083,0:34:16.500
can allow people
to build up a resilience toolkit.
0:34:17.500,0:34:22.791
And then there’s also responsibilities
that are more
0:34:22.791,0:34:26.541
so on
the workplace, are more so organizational.
0:34:28.000,0:34:30.041
Now on the on the level
0:34:30.208,0:34:33.500
of the research itself,
there’s a question for me
0:34:34.000,0:34:37.625
from those listening here
about the physicians that did the survey.
0:34:37.625,0:34:41.708
Were there many physicians
that that did the survey or what?
0:34:41.708,0:34:43.791
What sorts of people did you hear from?
0:34:43.791,0:34:44.333
Yeah.
0:34:44.333,0:34:47.833
So in terms of our demographic breakdown,
0:34:48.791,0:34:50.166
the majority
0:34:50.166,0:34:54.583
of the individuals that responded
to this particular phase of our study
0:34:55.416,0:35:01.708
were nurses, physicians
and personal support workers.
0:35:01.708,0:35:04.458
So that was generally
the biggest breakdown
0:35:05.583,0:35:07.958
with about 4% being physicians.
0:35:08.916,0:35:09.750
Okay.
0:35:09.750,0:35:11.833
And 51% being nurses.
0:35:13.000,0:35:14.000
Right.
0:35:14.916,0:35:18.750
This is an excellent question
that comes from our audience as well.
0:35:18.750,0:35:24.125
What is the role of education
in clinical ethics to build resilience?
0:35:24.750,0:35:25.875
Big question.
0:35:25.875,0:35:31.541
We don’t have a half an hour or an hour
or another symposium to answer it,
0:35:31.541,0:35:37.458
but what is the role of education
in clinical ethics in building resilience?
0:35:38.041,0:35:39.125
Mm hmm.
0:35:39.125,0:35:41.500
I think that’s such a great question.
0:35:41.500,0:35:44.583
And, you know, we’ve
we’ve had lots of discussions about that
0:35:44.583,0:35:46.958
in our our own team.
0:35:46.958,0:35:50.166
I think the one of the questions
0:35:50.166,0:35:52.750
that we asked in our interviews was,
0:35:53.166,0:35:58.458
have you ever received
education on mental health issues
0:35:58.458,0:36:02.208
for yourself as part of your training
as a health care provider?
0:36:02.208,0:36:07.125
And we’ve only had a very small handful
of people who’ve responded that they had.
0:36:07.125,0:36:10.958
So I think that speaks to the
broader need for education,
0:36:11.916,0:36:12.666
for health care
0:36:12.666,0:36:15.041
providers, about mental health period,
0:36:15.708,0:36:19.125
about taking care of their own mental
health, about the types of exposures
0:36:19.125,0:36:22.500
that they’re going to face
as a health care provider,
0:36:23.333,0:36:27.250
and how to help build some of those skills
0:36:28.083,0:36:32.375
to actually take care of themselves,
how to balance that
0:36:32.375,0:36:36.541
with the need to patient care
with their own self care.
0:36:36.833,0:36:41.291
And then just to learn about mental health
for themselves overall.
0:36:41.875,0:36:44.916
And in terms of ethics,
0:36:44.916,0:36:49.375
what we’ve heard a lot about is health
care providers have talked about
0:36:49.833,0:36:53.291
really wanting
a debriefing in the workplace.
0:36:53.791,0:36:56.958
So this would be
where there’s an opportunity.
0:36:57.250,0:37:01.958
Maybe there’s been a specific issue
or challenge in the workplace
0:37:02.375,0:37:08.166
that is causing you some tension
or feeling that moral sort of distress
0:37:08.166,0:37:13.083
in some way and that you have the ability
to come together as a group or a team,
0:37:13.208,0:37:16.541
you know, with your own team
or even bringing in some outside
0:37:16.750,0:37:20.000
supports into really sort of unpack that.
0:37:20.375,0:37:24.875
And the purpose of it is to kind of share
your own thoughts
0:37:24.875,0:37:29.208
and feelings about that issue
and how it impacted you personally
0:37:30.958,0:37:32.125
beyond sort of the
0:37:32.125,0:37:38.166
broader sort of,
I guess, patient care issues.
0:37:38.166,0:37:39.875
But it’s about turning that inward
0:37:39.875,0:37:43.416
to look at
how did that issue impact me specifically?
0:37:43.958,0:37:47.166
So that’s one of the things we’ve heard
quite a bit about, is that request
0:37:47.416,0:37:51.291
in all types of health care
settings, acute care, community
0:37:51.291,0:37:54.791
care, long term care, overall demeanor.
0:37:55.333,0:37:55.791
Yeah,
0:37:55.791,0:37:59.625
I just think that’s such a good point
about the debriefing and the connection,
0:38:00.541,0:38:03.458
because when I was talking
about resilience on a personal level,
0:38:03.750,0:38:04.916
I mentioned connection
0:38:04.916,0:38:07.750
going out and seeking it
and this is a perfect example of how
0:38:07.958,0:38:11.625
the distinctions
between organizational and personal
0:38:11.958,0:38:14.791
aren’t always very clear cut
0:38:14.791,0:38:17.708
because connection does help
build personal resilience,
0:38:17.708,0:38:21.625
but it’s also something
that the organization can support by
0:38:21.875,0:38:22.708
essentially building it
0:38:22.708,0:38:26.541
into the programing, building into the
culture, into the protocols.
0:38:27.500,0:38:30.208
So I think that was a great point
and a great response.
0:38:30.208,0:38:31.625
Ken, thank you.
0:38:31.625,0:38:32.375
Yeah, thank you.
0:38:32.375,0:38:32.958
Thank you.
0:38:32.958,0:38:35.583
Thank you. To the both of you
for this presentation.
0:38:35.583,0:38:39.541
It really is it’s impossible
to measure the importance of
0:38:40.500,0:38:44.916
of having not just the research,
but now as we move into this
0:38:45.208,0:38:49.625
this this next portion of the symposium
of attaching real faces to it.
0:38:49.625,0:38:51.875
But thank you, Mina and Kim, for this.
0:38:51.875,0:38:55.666
This has been fantastic stick
and I’m sure we’ll be going back to this
0:38:55.666,0:38:59.791
as we continue this symposium today.
0:38:59.791,0:39:03.958
As I said, names and stories adding
the names and stories to the research
0:39:03.958,0:39:06.541
we are exploring today. Very important.
0:39:06.875,0:39:10.833
So right now we are so fortunate
to have three health care professionals
0:39:10.833,0:39:14.375
with us to not only share
their experiences, but to also tell us
0:39:14.375,0:39:19.208
about what has helped and or hindered
their ability to care for themselves.
0:39:20.166,0:39:21.666
Aram Chagall.
0:39:21.666,0:39:24.958
Chagall is an emergency, and trauma nurse.
0:39:25.458,0:39:29.916
David Tabb is a physical therapist
in general and thoracic surgery,
0:39:30.208,0:39:33.750
and Todd
Tran is an occupational therapist.
0:39:33.750,0:39:37.916
I welcome
all three of you to the symposium today.
0:39:37.916,0:39:40.416
Hello.
0:39:40.416,0:39:42.333
Hello. Hi.
0:39:42.333,0:39:44.416
Thank you so much for having me here.
0:39:44.416,0:39:46.500
Thank you, Aaron. Thank you, Todd.
0:39:46.875,0:39:47.833
I agree with you.
0:39:47.833,0:39:49.125
I know you are.
0:39:49.125,0:39:51.625
David, great to see you as well.
0:39:53.291,0:39:53.708
Can I?
0:39:53.708,0:39:57.708
I think it’s always
the origin story is just so important
0:39:57.708,0:40:02.375
because it kind of sets the table
as to why you’re
0:40:02.583,0:40:06.583
why you’re here today speaking
and why are do why you do what you do.
0:40:06.583,0:40:09.666
So can you, each of you
briefly give us kind of like the Coles
0:40:09.666,0:40:12.958
notes of what drew you to your profession?
0:40:12.958,0:40:17.791
And I will start with you, Arab. So
0:40:18.875,0:40:20.083
I had actually been through
0:40:20.083,0:40:22.208
a lot in my life previously,
0:40:23.166,0:40:25.625
and I would say that
0:40:25.625,0:40:30.583
going into nursing was something
I wanted to do to help others.
0:40:30.583,0:40:34.833
But I would also say it
was the heavy influence of my late father
0:40:35.708,0:40:38.250
because he thought that I could
0:40:38.250,0:40:40.958
and thought that I had the potential
to help people in need.
0:40:41.833,0:40:44.041
Yeah, Yeah.
0:40:44.041,0:40:46.291
Todd, what about you? Hmm?
0:40:48.583,0:40:51.750
My story is more about going into
the health care field
0:40:51.750,0:40:56.458
because I was really interested
in the biological sciences in high school,
0:40:57.041,0:41:00.541
and not to date myself,
but in high school.
0:41:00.541,0:41:06.000
Back then we had a great 13,
and those 15 was called OEC,
0:41:06.000,0:41:09.000
and I took biology and really enjoyed it.
0:41:09.000,0:41:13.541
And physical education,
which I really loved about the health
0:41:14.583,0:41:17.000
perspective and chemistry was so-so.
0:41:17.000,0:41:18.708
But then comes physics. Not so.
0:41:18.708,0:41:24.958
So I, I fell in love with nursing
and which I did my first degree in.
0:41:24.958,0:41:29.041
But Then I switched over to occupational
therapy because I love rehab so much so.
0:41:29.375,0:41:35.375
And in a similar vein of helping
and contributing to society.
0:41:35.375,0:41:37.291
Yeah. Yeah.
0:41:37.291,0:41:39.500
And you, David?
0:41:39.500,0:41:42.291
Well,
I grew up in a in a health care family,
0:41:42.333,0:41:45.375
so my mother worked in health care
as a nurse and hospital administrator.
0:41:45.375,0:41:49.708
So I grew up around in that environment
and certainly spent quite a bit of time
0:41:49.708,0:41:50.916
volunteering at hospitals
0:41:50.916,0:41:55.000
when I was young with, you know, physios
and occupational therapists.
0:41:55.000,0:41:59.750
And I had to take a big role
in caring for my grandmother post-stroke.
0:41:59.958,0:42:03.250
So my or certainly my early experiences
really
0:42:03.666,0:42:06.833
kind of pushed me towards
physio as a career and I just wanted to,
0:42:07.208,0:42:11.125
you know, have a job that had a positive
impact on people’s lives. MM
0:42:13.708,0:42:16.125
So I want you all to take me back
0:42:16.291,0:42:19.416
to the early days of the pandemic
0:42:19.958,0:42:23.125
and what you were experiencing
0:42:23.125,0:42:27.375
at your place of work
as the pandemic began
0:42:27.375,0:42:29.791
to unfold
0:42:30.625,0:42:34.958
as really frontline workers,
you saw what was happening.
0:42:35.291,0:42:38.125
Can you just take me back to that
and what you were seeing
0:42:38.125,0:42:42.125
and what what might have been going
through your mind at the time?
0:42:43.166,0:42:45.083
I’ll start with you, Todd.
0:42:45.083,0:42:47.791
Sure.
0:42:47.791,0:42:53.166
As your bring me back to the early phase
of the pandemic, it was a lot of chaos.
0:42:53.166,0:42:55.416
That’s the word
that comes to mind right now.
0:42:55.416,0:43:00.750
And I laugh at it, but it became more
organized throughout the week, the waves.
0:43:01.333,0:43:04.833
But it was quite chaotic
because we were redeployed
0:43:05.250,0:43:08.916
from where I work in primary
care to a variety of roles,
0:43:08.916,0:43:12.875
from screening to working in the pharma,
in the pharmacy,
0:43:12.875,0:43:16.833
of drawing of the vaccinations,
to giving out the vaccines.
0:43:16.833,0:43:20.041
So it was chaotic in terms of
0:43:20.041,0:43:23.125
we don’t know where we were deployed.
0:43:24.458,0:43:27.833
We didn’t get a sense of autonomy
either in terms of people
0:43:27.833,0:43:31.750
asking in the leadership team
of like Todd, there’s a variety of rules.
0:43:31.750,0:43:34.916
Which one
would you like to give options or choice?
0:43:34.916,0:43:36.000
There was a lack of that.
0:43:36.000,0:43:40.000
It was more, you’re doing this
and you’re going to do this next.
0:43:40.583,0:43:45.375
And even when I was wanting to contribute
and be in a vaccine clinic
0:43:46.083,0:43:50.708
going the hotspots of Toronto,
we didn’t know
0:43:51.541,0:43:55.625
from week to week where we were going
in terms of hotspots and it wasn’t shared.
0:43:55.625,0:43:58.125
And our roles wasn’t given.
0:43:58.125,0:44:01.541
So it was really chaotic.
0:44:01.541,0:44:04.625
But again,
it became more organized along the way.
0:44:04.625,0:44:09.833
But initially I just wish
that people had more choice in the matter
0:44:09.833,0:44:14.708
and also to ask a variety of health care
workers, is it okay if we do this?
0:44:14.916,0:44:18.416
Are you immunocompromised because
we didn’t have any vaccines at the time?
0:44:18.875,0:44:22.583
Are you okay to be in the front line
to screen or to do such and such?
0:44:22.625,0:44:24.333
Or another question would be,
0:44:24.333,0:44:28.000
Are you living with anyone else
in your family that’s immunocompromised?
0:44:28.416,0:44:32.958
That conversation would have been lovely
at the initial phase versus not.
0:44:33.666,0:44:35.041
Yeah, yeah.
0:44:35.041,0:44:40.125
We will hear a little bit more about that
and what was what was happening
0:44:40.125,0:44:45.291
with you in the emergency room,
in the trauma centers.
0:44:45.541,0:44:53.708
What did it the those early days
of the pandemic look like?
0:44:53.708,0:44:54.875
I would say crazy.
0:44:56.125,0:44:58.208
You didn’t really have time to think.
0:44:59.583,0:45:02.041
You people being rolled in by EMS
0:45:02.041,0:45:07.000
stretchers one by one, one by one,
you would get calls in advance
0:45:07.000,0:45:09.958
saying that we have a cardiac arrest
because they were short of breath.
0:45:11.333,0:45:14.250
We had to get people on life support.
0:45:14.250,0:45:17.916
Within 5 minutes of arriving.
0:45:17.916,0:45:20.958
We barely had bed accommodation space.
0:45:20.958,0:45:23.041
We had to make some very hard decisions.
0:45:24.000,0:45:26.458
ICU was became jam packed.
0:45:26.458,0:45:29.250
We were outsourcing or
0:45:30.333,0:45:33.375
sending patients off
to other hospitals in different regions.
0:45:34.625,0:45:38.291
It was heartbreaking
to speak with families on the phone
0:45:38.791,0:45:41.791
who couldn’t be there
physically in the presence of their family
0:45:41.791,0:45:44.500
or their loved one who was dying
0:45:46.083,0:45:48.958
to hear them on the phone, to see them on
face time
0:45:49.208,0:45:52.500
was probably the only way that they could
communicate with their families.
0:45:54.291,0:45:55.083
We saw all
0:45:55.083,0:45:59.208
age groups get very ill,
and I would say that
0:45:59.208,0:46:03.416
there was absolutely no time
to think information was so ever evolving.
0:46:03.416,0:46:07.583
When you were triaging, it was like
you were trying to update yourself
0:46:07.791,0:46:11.833
day to day basis, hour to hour basis
in terms of what we were screening for.
0:46:12.458,0:46:16.791
At times, we were even to deploy from the
emergency department to screening centers
0:46:17.166,0:46:21.500
and we were triaging up to maybe
5 to 600 people in a day
0:46:22.041,0:46:27.583
that may have been exposed or had symptoms
that may have not even been covered.
0:46:27.583,0:46:32.041
But just because it was such it’s
such a novel disease that you had no idea
0:46:32.666,0:46:35.041
what symptoms could arise.
0:46:35.041,0:46:37.000
And I would say
0:46:38.583,0:46:41.500
The Unforgettable was also
0:46:41.500,0:46:43.375
how many bodies we had to beg
0:46:43.375,0:46:47.333
and sent down to the morgue.
0:46:47.333,0:46:51.875
That was that was what COVID
started as and continue does.
0:46:53.250,0:46:54.125
Yeah.
0:46:54.833,0:46:59.583
And you know, Todd spoke
about being redeployed and and folks
0:46:59.625,0:47:03.500
in different jobs found themselves
0:47:04.500,0:47:07.541
doing things
that they would never have imagined.
0:47:08.166,0:47:13.000
Like,
you know, taking care of the deceased.
0:47:14.041,0:47:17.583
David, you were also redeployed
0:47:17.583,0:47:21.666
during during the pandemic
in those early days.
0:47:21.666,0:47:23.583
What was going on for you?
0:47:23.583,0:47:26.250
Like, how were you
0:47:27.208,0:47:29.166
how were you processing,
0:47:29.166,0:47:33.750
what was happening,
the chaos that Todd and Aram talk about
0:47:33.750,0:47:37.291
and being redeployed, all of those things?
0:47:37.291,0:47:37.958
Well, it was
0:47:37.958,0:47:40.791
it was certainly very challenging
within the health center itself.
0:47:40.791,0:47:45.458
It was like Todd was saying,
just a very chaotic novel virus.
0:47:45.458,0:47:47.708
We didn’t have much information about it.
0:47:47.708,0:47:50.708
Even being able to judge
like my own personal risk
0:47:50.916,0:47:53.666
to the virus just with other
kind of health care factors,
0:47:54.500,0:47:57.666
with my regular job
being in orthopedic and general surgery,
0:47:58.625,0:48:01.750
Like we stopped
a lot of a lot of the elective surgeries.
0:48:02.041,0:48:06.083
So I was seconded to work in the ICU
for for quite a while.
0:48:06.541,0:48:09.916
And, you know, I do have ICU experience
and I’m used to working
0:48:09.916,0:48:13.333
with those level of patients,
but kind of being able to prepare myself
0:48:13.333,0:48:16.958
for the symptoms
and just the unique level of care that
0:48:17.166,0:48:19.750
those patients
with severe COVID pneumonia required
0:48:20.500,0:48:23.250
was challenging and there was really
no preparation for that.
0:48:23.250,0:48:26.416
I mean, you just had to know
you’re working with a novel virus.
0:48:26.416,0:48:27.875
It’s hard to kind of do
0:48:27.875,0:48:31.583
the best of your ability
and using good, sound clinical judgment,
0:48:32.875,0:48:36.000
it was certainly
it was even more challenging for myself
0:48:36.000,0:48:39.125
when we went to the ICU was
we weren’t just doing day shifts.
0:48:39.125,0:48:42.416
So we were kind of just because
of a lack of staff in general.
0:48:43.250,0:48:47.208
So we had to do 24 hour shifts
like 24 hour coverage
0:48:47.708,0:48:51.958
with very little of time
to to really accommodate to the
0:48:53.125,0:48:53.291
well,
0:48:53.583,0:48:57.541
just going from day nights and actually
little like maybe having one day
0:48:57.541,0:49:01.833
in between to accommodate from from night
to from night to day and so forth.
0:49:02.291,0:49:03.833
And that was certainly challenging.
0:49:03.833,0:49:07.125
I have a lot of newfound respect
for our colleagues
0:49:07.291,0:49:10.125
that they do that on a on on, on a normal.
0:49:10.625,0:49:12.791
But that certainly left me
in the situation.
0:49:12.791,0:49:14.666
I was say, you know, trying to cope with
0:49:14.666,0:49:18.250
just a stressful situation
of change, a job, a job, but then also
0:49:18.250,0:49:22.041
having to do it without with, you know,
like sleep deprivation and
0:49:22.625,0:49:26.875
and certainly not having my other avenues
for for health care.
0:49:27.791,0:49:28.583
You know, a lot of the care
0:49:28.583,0:49:32.458
I was having to provide was, you know,
a little out of scope of practice.
0:49:32.583,0:49:34.000
You know, there is limited things.
0:49:34.000,0:49:37.500
A lot we could do from a mobilization
standpoint with with patients.
0:49:37.958,0:49:41.791
But, you know, having to,
you know, help bag bodies,
0:49:42.125,0:49:45.375
you know, speaking to families bringing
them in in the middle of the night
0:49:45.666,0:49:48.458
to be able
to kind of say goodbye to their loved ones
0:49:48.458,0:49:51.291
with us was certainly challenging.
0:49:51.708,0:49:53.041
And a little another thing
0:49:53.041,0:49:57.250
that also made it tougher was,
you know, a lot of different professions.
0:49:57.250,0:50:01.541
Certainly received some, you know,
kind of, you know, acknowledgment
0:50:01.541,0:50:05.333
from the government and monetary supports
through pandemic pays.
0:50:05.708,0:50:10.000
But, you know, physiotherapists were
one of the one of the groups that didn’t.
0:50:10.000,0:50:14.416
So now there we are,
six of us, around a patient Proning,
0:50:14.416,0:50:18.833
a intubated patient,
and only one of the only one of us was not
0:50:18.833,0:50:24.291
getting kind of any monetary support saw
or through that with the pandemic pay.
0:50:24.791,0:50:28.791
So that was that was just kind of
knocked it down a little bit further.
0:50:29.375,0:50:30.958
Mm hmm. Mm hmm.
0:50:30.958,0:50:35.083
It speaks to the the moral injury
that that we’ve that we’ve
0:50:36.916,0:50:38.791
alluded to.
0:50:39.541,0:50:41.041
Was there a moment for
0:50:41.041,0:50:44.791
for each of you
when you started to feel that
0:50:45.125,0:50:51.333
that feeling of we’re in a place
now that we’ve never been to and
0:50:51.333,0:50:57.041
and you start to feel the personal risk of
of where
0:50:57.041,0:51:01.208
we were in the pandemic, where you were
in the work that you were doing.
0:51:01.458,0:51:05.250
Was there a moment
that that you can think of,
0:51:05.250,0:51:09.083
but were that sort of the tides turned?
0:51:09.125,0:51:10.833
Let’s call it that.
0:51:10.833,0:51:13.458
I’ll start with you, Todd.
0:51:13.458,0:51:15.875
And I think that’s a great question.
0:51:15.875,0:51:19.916
It’s a great question because there’s
multiple times that I felt that way.
0:51:20.958,0:51:23.250
But I think it to me
0:51:23.250,0:51:27.750
is the tide that turned
was the convoy freedom protest
0:51:28.291,0:51:31.583
that really threw me off guard because
0:51:33.708,0:51:35.916
it because speaking from my experience
0:51:35.916,0:51:42.833
as a double minority, as a Asian man,
but also as a gay man,
0:51:42.833,0:51:46.125
two of those narrative that I have
0:51:46.125,0:51:50.791
is going down to to psychological safety
because of COVID
0:51:50.791,0:51:55.000
being Asian,
it’s not a good time to be Asian.
0:51:56.666,0:51:58.458
And then on top of that, being a gay man.
0:51:58.458,0:52:00.625
But then the third thing
that really came on
0:52:00.625,0:52:04.625
board was the convoy freedom protest,
that they were coming to Toronto
0:52:04.625,0:52:08.500
on a particular weekend,
and the messaging from my organization
0:52:08.500,0:52:13.166
was do not wear identify yourself
0:52:13.166,0:52:17.541
as a healthcare worker
just because you might be targeted.
0:52:18.041,0:52:21.333
So that was a really turning point
where it’s like
0:52:21.333,0:52:25.500
what is going on in the state of the world
where there’s three hats
0:52:25.791,0:52:29.208
that that I have three identities,
three identities, and
0:52:29.208,0:52:33.500
I can’t show all three perhaps, or it’s
not safe to have those three identities.
0:52:33.500,0:52:36.875
So psychological safety was really
0:52:38.375,0:52:42.291
at the foreground for me
in my experience during that time.
0:52:42.833,0:52:45.416
And that’s a new social phenomenon.
0:52:45.458,0:52:48.250
That’s it’s
a triple minority. Right. Where
0:52:49.583,0:52:50.625
do you feel safe?
0:52:50.625,0:52:52.250
Can you be yourself?
0:52:52.250,0:52:55.625
It’s a feeling of hiding oneself during
0:52:55.625,0:53:00.000
this pandemic was really interesting,
which highlighted that.
0:53:00.000,0:53:03.125
So that was a really take away
where it’s like
0:53:03.125,0:53:05.250
what is going on
in the state of the world.
0:53:06.333,0:53:09.958
I think that was just from a layperson’s
perspective.
0:53:09.958,0:53:12.875
That was a real turning point
for many people watching
0:53:13.791,0:53:18.291
The fact that you were unable to
when when those messages were going out
0:53:18.291,0:53:22.000
that don’t identify yourself
as a health care worker,
0:53:22.208,0:53:26.458
when, you know, four months
prior to that were standing out
0:53:26.458,0:53:30.458
and banging pots and pans for health care
workers.
0:53:30.458,0:53:32.708
So, Erin, what about you?
0:53:32.708,0:53:36.958
Was there a
I know that you experienced something
0:53:37.750,0:53:40.625
very traumatic during a
0:53:41.500,0:53:44.833
during the pandemic
and having your father being hospitalized
0:53:44.833,0:53:48.083
and coming into the same hospital
that you worked
0:53:48.083,0:53:51.666
at as a COVID patient?
0:53:51.666,0:53:54.333
I mean, I can’t even call that
a turning point.
0:53:54.333,0:53:58.000
Can you tell us just a little bit
about that and how you were
0:53:59.791,0:54:03.250
processing that situation?
0:54:07.833,0:54:08.791
My heart dropped
0:54:08.791,0:54:16.083
into my stomach.
0:54:16.083,0:54:20.291
Watching people struggle to breathe
and die is a very difficult thing
0:54:21.750,0:54:24.666
when you see it happen
to someone that you know and love
0:54:25.416,0:54:31.833
makes it much more difficult.
0:54:31.833,0:54:35.708
I would say continuing
to work on the front line while my father
0:54:35.708,0:54:40.291
was hospitalized in the ICU was a way
for me to be connected with him
0:54:40.291,0:54:44.666
physically and spiritually
at every point in my life at that time,
0:54:45.500,0:54:48.541
because I really believe
that was his journey.
0:54:48.541,0:54:51.708
But it was also part of my
0:54:52.416,0:54:55.000
it was me working 12 hour
0:54:55.000,0:54:58.750
shifts or more
and then walking over to the ICU
0:54:58.750,0:55:02.583
just to see what was going on, getting
0:55:03.000,0:55:05.125
feeling frantic, getting phone calls.
0:55:05.875,0:55:09.250
I think it was
also very difficult at times
0:55:10.916,0:55:13.625
hearing a code blue alarm go off up
above in the
0:55:13.625,0:55:16.125
and the announcement in the hospital,
0:55:16.125,0:55:18.666
because naturally you would wonder
and think,
0:55:19.291,0:55:23.916
is that someone that, you know,
0:55:23.916,0:55:26.875
watching the news and really stressed out,
0:55:27.791,0:55:30.833
hearing about things such as you know,
0:55:30.875,0:55:34.916
new new laws and new decisions
0:55:34.916,0:55:38.708
that were being made about certain age
groups being taken off of life support
0:55:40.083,0:55:45.166
was very, very difficult for me.
0:55:45.166,0:55:47.333
But also to to add on to,
0:55:48.708,0:55:51.000
you know, what was mentioned
0:55:51.000,0:55:56.583
just now about the convoy protest
and then having patients come in and
0:55:56.583,0:56:02.291
and become irate and and physically
and verbally assaulting you in the E.R.
0:56:02.750,0:56:06.250
and to the point
where a lot of them did not want to mask
0:56:06.458,0:56:10.125
because they didn’t
really believe this disease was real
0:56:11.250,0:56:14.583
or refusing to get vaccinated
0:56:14.583,0:56:18.000
was something that really affected myself.
0:56:18.208,0:56:21.541
But I think it also impacted
a lot of my colleagues that worked with me
0:56:21.541,0:56:24.875
alongside with me,
because there were so many people
0:56:25.916,0:56:28.083
that would have really
wanted that vaccine.
0:56:29.416,0:56:33.375
But my father was one of them.
0:56:33.375,0:56:34.333
He was
0:56:35.833,0:56:40.000
he was to wait by one week.
0:56:40.000,0:56:41.583
And so
0:56:44.708,0:56:47.666
he then became ill
0:56:47.916,0:56:50.958
and ended up on life support
0:56:50.958,0:56:54.041
where he fought for his life
0:56:54.041,0:56:56.166
for the hardest month.
0:56:56.791,0:56:58.083
That was one hard month.
0:56:58.083,0:57:01.333
That was a very hard month.
0:57:01.333,0:57:03.625
So I would say that
0:57:03.625,0:57:07.458
there are there were so many people
that would have really wanted that vaccine
0:57:08.083,0:57:10.416
so that they could just have that chance
to live
0:57:12.541,0:57:14.458
and be alive.
0:57:14.458,0:57:18.458
And so many people that I’ve seen sick
just because they couldn’t get a vaccine.
0:57:19.625,0:57:22.625
And I think that’s what had angered me.
0:57:22.625,0:57:26.416
And and a lot of us felt
so angered about those who were.
0:57:26.416,0:57:29.708
And we do understand that
there’s questions that people have because
0:57:29.708,0:57:32.791
it’s such a new disease.
0:57:32.791,0:57:35.250
But can you imagine,
is that really worth your life
0:57:35.708,0:57:40.166
because so many people died
from not having that?
0:57:40.166,0:57:41.000
Yeah,
0:57:42.250,0:57:43.916
thank you for sharing that.
0:57:43.916,0:57:46.958
I know that this is not an easy topic.
0:57:46.958,0:57:51.208
And, you know, as we talk about risk
and resilience, this is still so fresh.
0:57:51.208,0:57:56.625
This is this these are not conversations
that are in the past.
0:57:56.625,0:57:59.583
They’re still happening now.
0:57:59.583,0:58:01.500
So thank you for that.
0:58:01.500,0:58:01.875
David.
0:58:01.875,0:58:05.791
I know that you’ve yourself had
0:58:07.083,0:58:09.083
some turning points and some questions
0:58:09.083,0:58:10.625
around
0:58:12.125,0:58:15.166
around what your role would be as
0:58:15.166,0:58:18.000
you were thinking about your family,
0:58:18.166,0:58:21.875
those outside
leaving the hospital, going back home.
0:58:21.875,0:58:28.416
I know that you and I spoke a little bit
about the difficulties of home life and
0:58:29.625,0:58:32.541
and all
of those those things that come with
0:58:33.625,0:58:34.833
the work that you do.
0:58:34.833,0:58:38.458
Can can you just get into that
just a little bit
0:58:38.458,0:58:41.916
of how how
0:58:42.125,0:58:43.833
your work kind of filtered
0:58:43.833,0:58:46.250
into into the rest of your life?
0:58:47.875,0:58:48.333
Certainly.
0:58:48.333,0:58:52.875
I mean, it was very challenging,
just not having or I think as I mentioned
0:58:52.875,0:58:58.375
before, or just the strategies
I would normally use for for self-care.
0:58:58.458,0:59:01.500
You know, we talked about friends
and family, you know,
0:59:01.500,0:59:03.833
being able to go out for dinners, travel,
0:59:04.625,0:59:08.708
you know, going to the gym, all regular
things that I would would certainly do.
0:59:08.708,0:59:10.458
So we’re dealing with a
0:59:10.458,0:59:13.083
very stressful situation
and having to cope with it
0:59:13.083,0:59:16.000
and isolation
and the sense that, you know,
0:59:17.166,0:59:20.166
the general public was told to,
you know, kind of stay with their family
0:59:20.166,0:59:21.083
is, you know, bubble
0:59:21.083,0:59:24.916
have that around you and then then isolate
if you had a potential exposure.
0:59:25.291,0:59:28.958
But when you’re dealing
with potential exposures on the daily
0:59:29.083,0:59:33.333
you know, certainly
no one wants to wants to be around you.
0:59:33.333,0:59:36.541
So you’re looked at as a hero and one
and then kind of one vain
0:59:36.541,0:59:40.000
and then certainly looked at as like
the virus when you’re out in the community
0:59:40.000,0:59:42.750
and know
just people being generally scared,
0:59:43.625,0:59:47.041
I really had to kind of shut down,
you know, and compartmentalize
0:59:47.041,0:59:48.708
any worrying thoughts that I that I had
0:59:48.708,0:59:52.583
for myself to be able to continue
to show up for work and
0:59:53.041,0:59:56.666
and to be able to to continue to advocate,
to help the public.
0:59:56.875,1:00:00.666
And also, I mentioned before,
just having that fatigue,
1:00:00.666,1:00:04.500
that of dealing with that on the daily
that when you come home not being
1:00:04.500,1:00:08.583
fully there for your for your spouse
or your significant other and
1:00:08.791,1:00:12.708
and also to help in
and there I’m mean not needs
1:00:13.291,1:00:14.583
and one thing that was also
1:00:14.583,1:00:18.583
was just having the responsibility
of you know working in the ICU with
1:00:18.875,1:00:22.083
you know patients you know on 200% oxygen,
you know, prior to,
1:00:22.750,1:00:26.375
you know, potentially being intubated,
you know, being one of the last
1:00:27.458,1:00:29.916
physical contacts that they might have.
1:00:29.916,1:00:33.375
I mean, family weren’t allowed to come in
and they weren’t allowed to do that
1:00:33.875,1:00:37.583
to see their loved ones
unless it was close to close to death.
1:00:37.583,1:00:40.291
And they were having to view them
through through an iPad.
1:00:40.416,1:00:44.791
So having that responsibility of,
you know, being actual human connection
1:00:44.791,1:00:48.166
to someone as they’re potentially
going through there, you know,
1:00:48.625,1:00:51.375
ending stages of life and,
you know, having to tell them,
1:00:51.875,1:00:55.416
you know, try to calm their anxiety that,
you know, things were going to be okay
1:00:55.416,1:00:57.916
when you really know that
that they’re not.
1:00:57.916,1:01:02.708
That’s an incredible and very weighing
responsibility to have had.
1:01:03.083,1:01:05.708
So yeah yeah
1:01:05.708,1:01:10.416
I wonder if the three of you have
1:01:10.416,1:01:13.000
had you know we just listened to the
1:01:13.750,1:01:18.416
the research on on resilience
and being able to kind of take the time
1:01:18.416,1:01:24.708
to build your resilience and to do
the things that are important for that.
1:01:24.708,1:01:28.833
And David, I think you, you outlined
many of those things very well.
1:01:28.833,1:01:32.791
You know, being able to work out
and see friends and family
1:01:32.875,1:01:35.750
be those things
that builds up your resilience,
1:01:36.541,1:01:39.166
have you all had the time
1:01:39.166,1:01:42.625
or the capacity
to be able to care for yourselves
1:01:43.750,1:01:44.833
during this time?
1:01:44.833,1:01:48.625
And and what are those things
that are your you’re holding on to?
1:01:48.625,1:01:51.708
Are those moments that you can hold on to
1:01:51.708,1:01:54.833
to keep you you going?
1:01:55.083,1:01:57.125
Aram, can I start with you? Is that okay?
1:01:57.875,1:02:00.750
Yes, that’s fine.
1:02:00.750,1:02:04.833
I would say for me, I’m
a very spiritually inclined person.
1:02:05.708,1:02:09.500
I really believe in a lot of power
and strength and meditation and prayer
1:02:09.666,1:02:12.166
and I really believe that is what
1:02:12.666,1:02:15.541
kept me going
through my very difficult times
1:02:16.000,1:02:19.500
while my father was hospitalized
when the pandemic
1:02:19.500,1:02:23.916
had even started,
1:02:23.916,1:02:26.291
I would say
that was something that kept me going
1:02:28.333,1:02:32.041
while my father was hospitalized
and I was working alongside with
1:02:32.041,1:02:36.333
other patients that were simultaneously
on life support as well.
1:02:36.958,1:02:41.250
And, you know, for me,
1:02:41.250,1:02:45.125
I feel like
that is a great resource of strength.
1:02:46.083,1:02:46.666
And that is
1:02:46.666,1:02:50.416
something that that kept me going.
1:02:50.416,1:02:54.000
The pandemic did have
a lot of restrictions in terms of
1:02:54.875,1:02:58.000
having to physically meet people,
1:02:58.125,1:03:01.250
speaking with people on the phone
or having anything virtual.
1:03:01.250,1:03:04.250
It was was,
I would say, a bit of a challenging issue.
1:03:05.166,1:03:07.250
And I would say that
1:03:07.416,1:03:11.833
on behalf of my colleagues, for instance,
because I think a lot of them
1:03:11.833,1:03:14.083
have been going through
so much personally,
1:03:15.708,1:03:18.083
each individual copes differently.
1:03:18.250,1:03:20.833
So the way that they
1:03:20.833,1:03:22.750
respond or react to stress
1:03:22.750,1:03:25.916
is going to be very vastly different
from each person.
1:03:27.083,1:03:30.541
I would also say a lot of other things
that kind of helped me
1:03:30.541,1:03:35.916
with coping were,
I would say, a lot of writing.
1:03:36.458,1:03:39.583
I’m very much into writing and to music
1:03:41.375,1:03:43.500
I like, you know, I
1:03:44.208,1:03:48.375
I’ve played a lot of musical instruments
and I would really feel like that was my
1:03:48.958,1:03:50.958
my circle or a space of Zen
1:03:51.875,1:03:55.500
for me too, to have that moment for myself
to really indulge
1:03:55.500,1:03:59.833
and just have that inner peace, to try
to align that inner peace within me.
1:04:00.833,1:04:01.750
Yeah.
1:04:02.458,1:04:04.416
How about you, Todd?
1:04:04.416,1:04:08.750
Have you had the the time,
the capacity to care for yourself?
1:04:08.750,1:04:11.416
And what have you been doing
1:04:11.416,1:04:12.666
for such a good question.
1:04:12.666,1:04:17.000
And when I reflect on that,
I really have to say I’m unsure
1:04:18.333,1:04:23.333
and sure, because being in the health care
system very I saw and witnessed
1:04:23.333,1:04:27.708
so many inequities that it’s just
it still sits with me, right?
1:04:27.708,1:04:31.208
You see it and you don’t know what to do.
1:04:31.208,1:04:34.750
And you’re experiencing
this moral distress or moral injury.
1:04:35.166,1:04:37.500
How do you heal from that?
1:04:38.583,1:04:40.541
Sure, sleep helps.
1:04:40.541,1:04:43.625
Taking time away helps,
but being in the health care system,
1:04:43.625,1:04:47.083
you’re kind of reminded, okay,
we need to make some change.
1:04:47.083,1:04:51.166
So I think that self-care is one thing.
1:04:51.166,1:04:54.791
But I also I would say it’s
the responsibility of the organization
1:04:54.791,1:04:59.916
as well to support us
after this experience because they did
1:04:59.916,1:05:04.833
such a great job as just putting people
together organized for deployment.
1:05:04.833,1:05:06.250
You cannot do this, do that.
1:05:06.250,1:05:11.333
But I think that same energy
needs to be deployed for management of
1:05:11.791,1:05:16.416
of such of how to take care of your team,
how to build back better,
1:05:16.791,1:05:22.750
how to promote a sense of mental
well-being in your team.
1:05:23.333,1:05:28.416
And just going back to the presentation
that we did was the organizational level
1:05:28.791,1:05:34.166
of perhaps being more transformative
leadership, promoting more sense of mental
1:05:34.166,1:05:40.375
well-being and supports
and really making that a priority somehow.
1:05:40.375,1:05:44.708
So I think it comes from within our self
to take care of yourself for sure,
1:05:44.708,1:05:50.833
but also coming from our organization
as well.
1:05:50.833,1:05:52.375
David do you feel like like
1:05:54.000,1:05:56.791
your supports, your organization is
1:05:56.791,1:06:00.958
is helping you along that that journey to,
1:06:02.583,1:06:07.000
you know, to give you back the capacity
to kind of take care of yourself or to,
1:06:07.333,1:06:10.791
you know,
are those systems in place for you?
1:06:11.791,1:06:14.208
Well, that’s that’s it’s it’s challenging.
1:06:14.375,1:06:17.750
I mean, although I’ve been able
to, you know, do some personal stuff
1:06:17.791,1:06:21.000
with regards to self-care, you know,
going back to, you know, being active,
1:06:21.000,1:06:24.916
working out,
I really certainly went to education
1:06:24.916,1:06:26.958
and to to really
1:06:26.958,1:06:30.333
to give myself some control,
like going to literature, learning about
1:06:31.000,1:06:34.750
the virus and with each and with each
new strand that was coming out.
1:06:35.083,1:06:37.916
And to give myself
a little bit of control in a
1:06:38.291,1:06:41.083
in an environment,
whether that were there was little.
1:06:41.083,1:06:43.625
It’s been challenging, though,
because, I mean, the state of our health
1:06:43.625,1:06:44.791
care system has gone.
1:06:44.791,1:06:46.333
We’ve gone from a COVID pandemic
1:06:46.333,1:06:50.541
to a pandemic staffing,
and that’s been challenging for us.
1:06:50.541,1:06:52.041
I certainly know that.
1:06:52.041,1:06:55.000
I know organizations,
you know, have job postings out
1:06:55.000,1:06:57.458
and have had them up for months and
and years.
1:06:57.875,1:07:02.625
But there’s very that, you know, we can do
when there’s just no people that that
1:07:02.666,1:07:03.666
that want to do the job.
1:07:03.666,1:07:07.875
And so now we’re moving from
you know, the our secondments
1:07:07.875,1:07:11.416
and dealing
with the severity of COVID itself.
1:07:11.416,1:07:16.750
And now we’re going into just an onslaught
of trying to clear the surgical backlogs
1:07:16.750,1:07:19.833
and the constant push to,
you know, try to move through quicker.
1:07:19.833,1:07:23.500
And, you know, and you’re also working
with more challenging,
1:07:23.500,1:07:24.666
you know, patients and families
1:07:24.666,1:07:28.000
who haven’t had the appropriate
level of care for the last 2 to 3 years.
1:07:28.000,1:07:31.291
And and doing that with the same,
you know, very same
1:07:31.291,1:07:34.416
level of staffing
that was that was there prior prior,
1:07:34.416,1:07:38.583
which has been limited
as certainly has been challenging.
1:07:38.583,1:07:39.500
And I know it’s something
1:07:39.500,1:07:43.500
that all organizations, you know,
are trying to are trying to correct.
1:07:43.500,1:07:44.166
It’s just,
1:07:44.166,1:07:47.583
you know, certainly difficult when there’s
just not enough of the skilled people
1:07:47.875,1:07:52.166
wanting to wanting to take the positions.
1:07:52.166,1:07:57.541
I have no doubt that this has been the most challenging period in your work lives,
1:07:59.083,1:08:01.375
but you’re still all still
1:08:02.791,1:08:06.500
you are still working, you’re
still getting up and going to your jobs.
1:08:06.500,1:08:08.416
And I wonder about
1:08:08.708,1:08:12.625
where Hope lies in all of this for you
and and
1:08:12.958,1:08:15.375
and why it’s important to just keep
1:08:15.666,1:08:18.083
on keeping on as you’re going
1:08:19.541,1:08:20.791
to. I
1:08:24.291,1:08:27.333
what keeps me going
is the connections that I make
1:08:27.333,1:08:32.041
with the people that I work with,
the clients, the patients
1:08:32.458,1:08:36.375
and my colleagues, because I realize that
that’s my second family.
1:08:36.666,1:08:40.791
I have my own family,
but it’s the work family.
1:08:41.250,1:08:46.208
And just going back to the first question
of why I went to the field, I loved the
1:08:46.500,1:08:51.250
the contribution
that I make to people’s lives,
1:08:51.250,1:08:53.750
and that keeps me going.
1:08:54.333,1:08:57.416
And also being curious
and being in the health care system.
1:08:57.416,1:09:00.291
How can I contribute
to make it more equitable?
1:09:00.291,1:09:03.250
Because I think it’s everybody’s
responsibility now,
1:09:03.291,1:09:07.000
not just the leadership team, but for me
now, after speaking COVID
1:09:07.500,1:09:13.500
I, the pandemic is I need to voice biases.
1:09:13.500,1:09:18.000
I need to communicate from
a bystander if things are
1:09:20.041,1:09:23.166
not ethical,
not equitable, that sort of thing.
1:09:23.166,1:09:26.875
So I think now
I have a different lens of going into this
1:09:27.750,1:09:31.041
from the next chapter of my life
and my career to
1:09:31.083,1:09:34.750
how can I make a positive influence
in a different way this time
1:09:35.250,1:09:40.583
so that we can learn from the endemic,
not make the same mistakes.
1:09:40.583,1:09:44.375
So coming from that angle is a strength
based focus
1:09:44.791,1:09:47.166
versus from a pessimistic
point of view of health care.
1:09:47.166,1:09:48.833
Because we can go there.
1:09:48.833,1:09:52.208
But I think I’m focusing more
on the strength of health care.
1:09:53.041,1:09:55.041
Yeah, with the.
1:09:55.916,1:09:56.708
Thank you for that.
1:09:56.708,1:09:58.000
What the few minutes we have.
1:09:58.000,1:10:00.000
What about you, David?
1:10:00.666,1:10:03.708
A what is what is keeping you in it
1:10:03.708,1:10:07.166
and giving you hope these days?
1:10:07.166,1:10:09.666
Well, as interestingly listening
to the talk about resiliency.
1:10:09.666,1:10:10.541
So I am getting older.
1:10:10.541,1:10:14.500
So my resiliency builds
certainly builds with age but
1:10:16.041,1:10:19.083
but no, it’s still coming back
to, you know, why
1:10:19.083,1:10:22.041
I went into the profession
in the first place and having that ability
1:10:22.416,1:10:25.833
to certainly help other people
and and and family.
1:10:25.875,1:10:28.750
I mean, my secondary job
that’s kind of popped up
1:10:28.750,1:10:31.750
has been a health care navigator
for friends and family in this time.
1:10:31.750,1:10:35.500
Just because our health care system is
certainly is very fractured
1:10:35.500,1:10:38.166
from from where it was before
and just trying to get to appropriate
1:10:38.166,1:10:41.083
levels of care
afterwards has certainly been challenging.
1:10:42.125,1:10:44.500
And I just really hope that, you know,
1:10:45.083,1:10:48.291
from a higher levels of government
that would that we learn from this,
1:10:48.291,1:10:49.833
you know, whether,
1:10:49.833,1:10:53.750
you know, everything was truly heated
after or after this virus pandemic.
1:10:53.750,1:10:57.125
And and in 2003 was was really carry
forward.
1:10:57.125,1:11:00.041
And, you know, there was a lot of a lot of
talk and a lot of questions about that.
1:11:00.750,1:11:03.625
So I really hope that, you know,
I hope that, you know,
1:11:03.625,1:11:08.083
we have good people in place
that can really push forward
1:11:08.083,1:11:12.125
and and really learn from this, you know,
try to support that on the front lines.
1:11:12.208,1:11:15.875
Certainly looking at staffing models,
not trying to do not trying
1:11:15.875,1:11:17.791
to do more with less. And I
1:11:19.291,1:11:20.500
have hopes that that will happen.
1:11:20.500,1:11:23.583
And we’ll just have to
just have to keep soldiering on.
1:11:24.500,1:11:26.500
Yeah for sure.
1:11:26.500,1:11:30.125
And you, Aram, what is giving you hope?
1:11:30.125,1:11:35.041
What’s keeping
you getting up and doing the work?
1:11:35.041,1:11:38.416
I would probably say that
1:11:38.500,1:11:40.625
we’ve all been
through such a difficult battle.
1:11:40.625,1:11:42.083
So why stop now?
1:11:42.083,1:11:42.875
Why what?
1:11:42.875,1:11:46.416
Why? Why would I stop now?
1:11:47.333,1:11:49.625
I would also say
1:11:49.625,1:11:53.916
that it is to continue the legacy
of my late father, because I know
1:11:53.916,1:11:56.541
it’s something that he really wanted me
to do and continue.
1:11:57.333,1:11:59.958
And I know that he wanted me.
1:11:59.958,1:12:02.458
And I know he always would say that.
1:12:02.458,1:12:04.875
I know that you will
1:12:04.875,1:12:07.750
shape
and change the world for a better place.
1:12:08.958,1:12:11.708
And I think lastly,
what I’d like to add on to
1:12:11.708,1:12:14.958
that is given this experience.
1:12:16.291,1:12:17.125
You know,
1:12:17.125,1:12:20.125
SaaS and Ebola, for example,
those were like our
1:12:21.875,1:12:23.250
our wake up calls.
1:12:23.250,1:12:27.833
And I think getting input from individuals
such as ourselves is what mistake
1:12:27.875,1:12:30.208
are we going to avoid for the future
1:12:30.208,1:12:33.208
and and try to implement programs,
for example,
1:12:33.208,1:12:37.083
such as emergency preparedness programs,
of what mistakes we made
1:12:37.083,1:12:40.333
and what things could be done
better, implementing
1:12:41.458,1:12:44.375
programs and mental health
awareness programs and support
1:12:44.375,1:12:47.083
groups for health care
workers at the start of the pandemic.
1:12:47.458,1:12:49.208
It’s long overdue.
1:12:49.208,1:12:51.416
And you know, things like that.
1:12:51.416,1:12:55.000
For example,
because so many lives have been lost.
1:12:55.000,1:12:57.541
And I just think that it could
just have been managed so much better.
1:12:59.125,1:13:01.333
But I would say that
1:13:01.333,1:13:03.666
to implement more, to implement
1:13:05.041,1:13:07.708
and shape the world into a better place
1:13:07.708,1:13:10.416
and just that change for a better
tomorrow.
1:13:11.041,1:13:12.500
Yeah.
1:13:12.500,1:13:14.916
Thank you all so, so much.
1:13:14.916,1:13:19.000
Aram and Todd and David
and I wish you the best
1:13:19.000,1:13:22.291
as you push forward and in care of us.
1:13:22.291,1:13:26.666
And I thank you for not just taking
this time and a symposium here, but
1:13:27.666,1:13:29.041
for the work that you do.
1:13:29.041,1:13:31.541
Thank you for being here today.
1:13:31.541,1:13:34.416
Much appreciated.
1:13:35.291,1:13:37.875
Hello. Welcome back, everyone.
1:13:37.875,1:13:39.333
I hope that
1:13:39.916,1:13:42.625
you had a short break
and you put it to good use.
1:13:43.333,1:13:46.750
We have learned
so in this in our morning session
1:13:46.958,1:13:50.708
in the in the early parts of the symposium
about risk and resilience through
1:13:50.708,1:13:53.791
the personal lens of our generous health
1:13:53.791,1:13:57.916
care and the panelists and
and through the data
1:13:57.916,1:14:01.500
and recommendations
coming out of the research,
1:14:02.708,1:14:06.375
I have to say that, you know,
I am learning so much about PTSD,
1:14:06.375,1:14:10.500
about moral injury
and risk and my own resilience.
1:14:11.875,1:14:17.583
But you I’d say that we do lean on on
1:14:17.708,1:14:22.208
you all the most
and at our most vulnerable times.
1:14:22.625,1:14:26.791
And so it’s good
to really take a step back and look at
1:14:27.250,1:14:30.250
what what we can do to help
1:14:30.541,1:14:34.208
to alleviate some of this this burden
and this this stress.
1:14:34.583,1:14:36.666
We’re going to continue this conversation
with colleagues
1:14:36.666,1:14:41.375
from the University of Alberta
who will present a tool called The Matrix
1:14:42.000,1:14:46.375
that aims to impart mood individuals
from NEG negative
1:14:46.375,1:14:50.458
psychological distress
or behaviors to more positive behaviors.
1:14:50.958,1:14:54.000
Dr. Suzette Brémault-Phillips and Dr.
1:14:54.250,1:14:55.083
Lorraine Smith.
1:14:55.083,1:14:58.833
McDonald can give you and give us
1:14:58.833,1:15:01.708
a bit of background on the Matrix.
1:15:01.916,1:15:03.000
I’ll turn it over to them
1:15:08.166,1:15:18.208
to then we go, Can everyone hear me?
1:15:18.208,1:15:19.625
Is it okay now?
1:15:19.625,1:15:21.625
Okay, wonderful. Sorry about that.
1:15:22.000,1:15:25.083
So I just wanted to say thank you
so much for that introduction
1:15:25.500,1:15:27.541
and we’re very to be here
1:15:28.083,1:15:30.666
and as already has been mentioned
in the symposium
1:15:30.666,1:15:34.000
many times, we just want to acknowledge
both the risk and the harm
1:15:34.000,1:15:38.125
that has come out of the pandemic,
whether that’s PTSD or moral injury
1:15:38.666,1:15:42.458
or just any of those other components
that people have had to experience.
1:15:43.625,1:15:47.375
But I think we also just want to honor
the moments, resilience that we just heard
1:15:47.375,1:15:51.500
about in the last presentation
and to just really speak to the fact
1:15:51.500,1:15:56.708
that as much as we know that risk comes,
so too can resilience come.
1:15:57.250,1:15:59.875
And we want to share a little bit
about our definition
1:15:59.875,1:16:04.166
of risk and resilience
and how we we believe you can build it.
1:16:05.416,1:16:08.041
And so I will turn it over to Dr.
1:16:08.041,1:16:09.708
Suzette Brémault-Phillips
1:16:09.708,1:16:13.541
to just give us a little bit
of an introduction about our understanding
1:16:13.875,1:16:17.166
of risk and resilience
before we move into the Matrix.
1:16:18.000,1:16:18.958
Thank you. Dr.
1:16:18.958,1:16:20.875
Seth McDonald It’s a pleasure being here.
1:16:20.875,1:16:23.041
Thank you everyone for the opportunity.
1:16:23.916,1:16:27.083
Yeah, well, there’s a lot of different
of models of resilience.
1:16:27.083,1:16:28.250
One way that we can look at it
1:16:28.250,1:16:31.666
is to think of resilience
and risk as two sides of the same coin.
1:16:32.250,1:16:35.083
On the one hand, harm
is anything that can challenge
1:16:35.083,1:16:38.375
our values external threat to us.
1:16:38.375,1:16:42.333
Yet at the same time, despite that threat,
we have the innate desire
1:16:42.333,1:16:45.500
in our hearts
to continue to move forward early on.
1:16:46.291,1:16:50.791
We hope, even if the glimmer of hope is
extremely small or hard to find sometimes.
1:16:51.458,1:16:54.875
But with time,
this harm can sometimes overcome our hope.
1:16:54.875,1:16:57.791
And so there’s a need to go deeper
to find a way to get through.
1:16:58.666,1:17:02.458
We posit that resilience
is about our values as well.
1:17:02.500,1:17:06.583
To be resilient, we need to know
what matters to us the most, i.e.
1:17:06.666,1:17:10.625
what our core values are and how we want
to live out those values in our lives.
1:17:11.416,1:17:15.125
If we don’t care about something,
it doesn’t align with our values or who
1:17:15.125,1:17:19.833
we want to be, then it’s going to be
very difficult to care or to carry on.
1:17:20.583,1:17:23.166
Knowing what matters to us
helps us to clarify
1:17:23.166,1:17:25.875
where we put our energies or what
things are worth fighting for,
1:17:25.875,1:17:29.166
and equally importantly,
what things we should let go of.
1:17:29.875,1:17:34.625
Resilience is about trying to, in small
steps, be able to realign with our values.
1:17:35.125,1:17:37.791
In difficult times, we often lose sight
1:17:37.958,1:17:42.583
of what we are trying to achieve
or why we’re doing things Left unchecked.
1:17:42.750,1:17:46.291
This can lead to helplessness,
feelings of hopelessness
1:17:46.625,1:17:49.875
which further compound
or can compound our sense of harm.
1:17:51.000,1:17:51.708
Taking small
1:17:51.708,1:17:54.125
steps to clarify what matters to us most,
1:17:54.750,1:17:58.125
However, it can provide us with greater
understanding and a clearer sense
1:17:58.125,1:17:59.666
of meaning and purpose
1:17:59.666,1:18:03.541
and a pathway to get through the harm
that we’re experiencing.
1:18:03.541,1:18:05.875
And that’s where resilience shines
the most.
1:18:06.250,1:18:09.000
So again, resilience is about our values.
1:18:09.208,1:18:11.458
What matters to us the most?
1:18:11.458,1:18:13.250
Act Hillary Great.
1:18:13.250,1:18:14.791
Thank you so much.
1:18:15.041,1:18:18.583
We also just want to acknowledge,
as has been discussed in this symposium,
1:18:18.583,1:18:22.125
that resilience is something
that is a joint responsibility
1:18:22.125,1:18:26.791
between ourselves and other people,
specifically employers and employees.
1:18:27.375,1:18:31.458
And employers need to make those changes
to be able to improve
1:18:31.791,1:18:35.291
workplace factors that reduce
mental health and promote resilience.
1:18:35.458,1:18:38.916
So we want to just acknowledge
before we get into the matrix specifically
1:18:39.291,1:18:43.750
that this tool, while being specific to
individuals, can be used on a team level
1:18:44.083,1:18:48.125
and can also be used in ways
to support this more global and more
1:18:49.333,1:18:51.375
societal approach to resilience.
1:18:52.625,1:18:55.250
So before anything else,
1:18:55.250,1:18:58.125
why don’t we jump right into the matrix?
1:18:58.333,1:19:01.750
This is a tool that was developed
by acceptance and commitment therapy,
1:19:02.000,1:19:05.666
and it’s an evidence based tool to try
and support people to move from risk
1:19:05.958,1:19:14.958
to resiliency.
1:19:16.333,1:19:19.333
Hi, We’re going to introduce you
to a tool called The Matrix.
1:19:19.750,1:19:21.375
The Matrix is a perspective.
1:19:21.375,1:19:25.291
It’s a way that we can look at things
and we can use the matrix, understand our
1:19:25.291,1:19:29.541
experiences and help guide our choices,
especially when we’re feeling stuck.
1:19:29.541,1:19:31.791
It can help us
figure out how to get unstuck.
1:19:32.083,1:19:34.166
So the Matrix has two axes.
1:19:34.166,1:19:38.500
The first is towards in a way,
and this means towards
1:19:38.500,1:19:41.708
what matters to you, towards
who’s important to you, towards
1:19:41.708,1:19:45.208
your values, what’s important
and matters to you or away from
1:19:46.208,1:19:48.333
the other axes is inside and outside.
1:19:48.583,1:19:52.083
Inside is our internal
thoughts, feelings and sensations
1:19:52.083,1:19:54.750
and outside
is anything you can notice with your five
1:19:55.583,1:19:58.166
or your own behavior,
which is what other people can see.
1:19:58.166,1:19:59.166
You two
1:19:59.708,1:20:01.750
in the middle is us noticing,
1:20:01.750,1:20:04.791
hopefully
with some kindness and curiosity.
1:20:04.791,1:20:08.166
And so it’s important
because it also helps us notice
1:20:08.166,1:20:11.625
what’s happening and to take a different
perspective of thinking about things,
1:20:11.708,1:20:15.375
not in terms of good,
bad, right, wrong, true or false,
1:20:15.666,1:20:18.958
but in terms of towards
what matters or away from what matters.
1:20:19.416,1:20:22.750
We can also use a matrix
to understand risk and resiliency.
1:20:23.333,1:20:27.458
So in a sense, risk is when we get stuck
on the away side of the matrix.
1:20:27.708,1:20:31.083
As humans, we often do things
that are short term solutions
1:20:31.291,1:20:33.458
but end up costing us in the long term
1:20:34.625,1:20:38.458
resiliency is then getting to the towards
side of the matrix.
1:20:38.458,1:20:41.833
It means that we’re doing things
that are important to us,
1:20:42.000,1:20:45.000
that matter to us
even when things are difficult.
1:20:46.291,1:20:49.708
And our goal is simply to move
a little bit more towards than away.
1:20:50.041,1:20:53.875
Nobody can spend all their time
on the towards side of the matrix.
1:20:53.875,1:20:56.291
So now we’re going to use the Matrix.
1:20:56.291,1:20:58.583
And to give you an example
of how you can use it,
1:20:59.625,1:21:03.083
the now we’re going to go through
an example of how we can use the matrix.
1:21:03.083,1:21:04.583
In this example, Dr.
1:21:04.583,1:21:07.208
Jaimie and I are going to use the Matrix.
1:21:07.625,1:21:10.958
I’m going to be using an example
from my own personal experience.
1:21:10.958,1:21:14.125
I spent almost 15 years
on the medical surgical and cancer
1:21:14.125,1:21:18.041
care units at the hospital,
and I was there for part of the pandemic.
1:21:18.458,1:21:22.083
And so as a frontline worker working
in the cancer center during the pandemic,
1:21:22.125,1:21:23.083
I’m going to use my own
1:21:23.083,1:21:27.083
personal experiences to help us understand
how we can use the Matrix.
1:21:27.250,1:21:29.250
So let’s
see how we can make use of this tool.
1:21:31.041,1:21:31.625
Hey, Dr.
1:21:31.625,1:21:33.916
Dayna. Hey, Dr. Jaimie.
1:21:35.250,1:21:38.791
Let’s talk about something related
to your experiences as a health care
1:21:38.791,1:21:43.291
worker, especially the ways that you felt
stuck as a health care worker.
1:21:44.500,1:21:48.791
Yes. So I would say one of the parts
that was the most difficult
1:21:48.791,1:21:51.916
and I get the most stuck on where
some of the rules that really
1:21:51.916,1:21:55.041
it felt like they were putting patients
and health care providers at risk.
1:21:55.166,1:21:58.583
Sometimes those were government rules,
sometimes were institution rules
1:21:59.041,1:22:00.166
during the pandemic.
1:22:00.166,1:22:02.083
Sometimes it was about me.
1:22:02.083,1:22:04.875
And when you could get it
or how you should use it, other times
1:22:04.875,1:22:08.166
it was about when and where
and who was allowed to go
1:22:08.166,1:22:11.500
in and out of the hospital
and where you had to work.
1:22:11.500,1:22:15.000
And there was just constant worry
about bringing the virus either
1:22:15.000,1:22:18.791
in or out of the hospital, especially
at early stages of the pandemic.
1:22:19.375,1:22:21.000
Yeah.
1:22:21.000,1:22:23.208
So pain painful.
1:22:23.916,1:22:26.791
So I’m not I’m going to put this
on the matrix, Dr.
1:22:26.791,1:22:29.916
Dayna, away from what matters
because this pain was
1:22:29.916,1:22:33.375
really, really taking you away
from the things that mattered
1:22:34.083,1:22:37.000
and in the internal world. So
1:22:38.041,1:22:41.000
could you tell us a little bit
about those painful thoughts
1:22:41.166,1:22:44.916
and feelings and memories
that you had during that time?
1:22:46.041,1:22:48.791
Yeah,
there was a lot of anger and frustration.
1:22:48.791,1:22:51.500
And I would say
also really feeling helpless
1:22:51.500,1:22:54.250
and sometimes hopeless
that things weren’t going to change.
1:22:54.541,1:22:57.458
Sometimes we tried so hard
to get those roles to change
1:22:57.458,1:23:00.541
and sometimes we made no progress at all.
1:23:00.541,1:23:02.000
And I also heard you say
1:23:02.000,1:23:05.333
just memories of people, patients
and coworkers being harmed.
1:23:05.916,1:23:08.208
Yeah, it was really upsetting too.
1:23:08.208,1:23:11.375
You know, we all get into profession
because we want to help people.
1:23:11.375,1:23:12.875
And here there are these roles
1:23:12.875,1:23:16.416
that feel like they’re harming
both patients and our coworkers.
1:23:16.833,1:23:18.333
So thoughts like what?
1:23:18.333,1:23:21.333
What was going through your head like,
this is unfair.
1:23:21.333,1:23:23.916
I need to fix this. Why is this happening?
1:23:24.791,1:23:27.791
Any any body sensations
with all this pain?
1:23:28.416,1:23:32.458
Oh, well, like constant tension
just all the time.
1:23:32.875,1:23:33.666
Mm hmm.
1:23:33.875,1:23:37.625
Okay, so lots of anger,
lots of frustration.
1:23:37.625,1:23:40.583
Helpless, hopeless Great noticing.
1:23:42.125,1:23:44.583
All right, so we’re going to move up here.
1:23:44.583,1:23:49.083
So this is away from what matters
and what people see in the outside world.
1:23:49.083,1:23:52.541
What what did you do to move away
from this pain?
1:23:54.083,1:23:58.291
Well, I would say we often
got into arguments with management
1:23:58.291,1:24:01.458
trying to get people to change
or to convince people,
1:24:01.458,1:24:04.875
you know, of the importance
of how things needed to be different.
1:24:05.541,1:24:07.166
That was a big thing.
1:24:07.166,1:24:11.750
So what else did you do when you felt
frustrated, hopeless, helpless?
1:24:12.625,1:24:13.125
Yeah. I mean,
1:24:13.125,1:24:17.166
we often didn’t get anywhere with that,
so we did feel like super hopeless.
1:24:17.166,1:24:21.250
I’m I’m pretty I was like pretty snappy
with my family members.
1:24:22.416,1:24:27.000
And I probably started to, like,
avoid some of my friends because they just
1:24:27.000,1:24:31.375
didn’t want to keep hearing about
all of our stressors at the hospital.
1:24:32.250,1:24:33.083
Yeah.
1:24:33.250,1:24:37.291
So what happens
is this these thoughts and feelings
1:24:38.541,1:24:41.375
in their way Internal.
1:24:41.375,1:24:45.666
You started coping with them
with these away outside, right?
1:24:46.000,1:24:50.583
Is there anything that happened
as a result of these away outside moves
1:24:50.583,1:24:53.041
like so while you’re getting in arguments
with management,
1:24:53.416,1:24:57.000
trying to get people to change,
getting snappy, avoiding friends,
1:24:57.000,1:25:00.583
what painted that ad on the inside?
1:25:01.833,1:25:04.541
Well,
I end up just feeling even more frustrated
1:25:04.541,1:25:07.333
and angry
because you can’t get them to change
1:25:08.375,1:25:10.541
and then you start
to feel like a horrible person
1:25:10.541,1:25:13.500
because you’re not,
you know, hanging out with your friends
1:25:13.500,1:25:16.625
and you’re being snappy
and difficult with your family.
1:25:16.625,1:25:17.375
Like,
1:25:18.333,1:25:20.500
Yeah, okay, so
1:25:21.875,1:25:26.541
great noticing and notice
what’s starting to happen.
1:25:26.541,1:25:32.375
These away inside
experiences are contributing to these away
1:25:32.375,1:25:37.625
outside actions which are then
leading to more a way outside experiences.
1:25:37.833,1:25:42.875
So we start to spiral on this side
and when people come to us stuck,
1:25:43.250,1:25:44.583
they can be
1:25:44.583,1:25:48.875
in a in a high risk situation
where they’re spiraling on this away side.
1:25:49.708,1:25:53.000
So when we get fixated on this away
1:25:53.000,1:25:56.791
side of the matrix,
the pain and the ways managing the pain
1:25:58.541,1:26:00.916
and then trying to get rid of these
1:26:01.500,1:26:05.458
as if somehow if we worked hard enough,
we could get rid of them.
1:26:05.458,1:26:08.750
We can stay just in this spin.
1:26:09.541,1:26:13.208
So, so we’ve all been there
trying to get rid of these things
1:26:13.208,1:26:16.458
and we know what we’ve learned
can’t be unlearned.
1:26:17.041,1:26:19.625
And even if we could get rid
of all this stuff,
1:26:19.958,1:26:23.333
it still isn’t getting us over here
to the things that matter to us.
1:26:23.875,1:26:29.041
So where we’re really focusing
now is moving to this towards side where
1:26:29.333,1:26:34.125
we’re living a meaningful, purposeful
life, connecting with what matters to us.
1:26:34.125,1:26:38.291
So let’s move over to this toward
the inside world of yours
1:26:38.583,1:26:42.000
with who or what matters to you.
1:26:42.000,1:26:43.875
Well, I would say obviously
1:26:43.875,1:26:47.208
my family and my friends matter to me.
1:26:48.666,1:26:50.416
You know, my
1:26:50.500,1:26:54.250
colleagues and patients,
they were important as well.
1:26:54.250,1:26:54.958
Okay.
1:26:55.000,1:26:56.750
So that’s who matters to you.
1:26:56.750,1:26:58.833
How about what matters to you?
1:26:58.875,1:27:01.125
What are some of those values
that matter to you?
1:27:02.083,1:27:05.166
Well, again,
I really got into this profession to,
1:27:05.166,1:27:08.250
like, help reduce human suffering,
to make things better
1:27:08.250,1:27:13.333
for people,
to help them live healthier, better lives.
1:27:13.333,1:27:17.625
When we think about these values
and we move up to this towards outside
1:27:18.250,1:27:21.250
part of the matrix for looking at
what could you do
1:27:21.500,1:27:24.333
to live out these values
and care for these people.
1:27:24.666,1:27:29.291
And one of the things you said
you’re trying to do is change the system,
1:27:29.708,1:27:33.083
help the system be more responsive, help
the system take care of health care
1:27:33.125,1:27:34.583
workers, patients.
1:27:34.583,1:27:37.458
And you tried that
strategy, it sounds like,
1:27:38.666,1:27:41.416
to to the end degree.
1:27:41.833,1:27:44.125
So that matters.
1:27:44.166,1:27:45.375
That matters.
1:27:45.375,1:27:49.250
And we’re also trying
to find other things up here
1:27:49.875,1:27:51.458
that would help you live out these values.
1:27:51.458,1:27:54.750
So when you think about these people
and these things that matter to you,
1:27:54.791,1:27:59.375
what else could you do to live out
the inside towards quadrant?
1:28:00.250,1:28:03.000
Well, I mean,
I guess I could definitely spend more time
1:28:03.000,1:28:07.000
with friends and family
and not be so grumpy around them.
1:28:07.583,1:28:09.666
Yeah, what else?
1:28:09.833,1:28:12.541
How about taking care of your colleagues
and patients?
1:28:13.291,1:28:16.416
Well, I mean,
I think it was probably really helpful
1:28:16.416,1:28:21.291
when we supported each other as colleagues
and just recognized how hard it was.
1:28:21.291,1:28:23.125
Often people who weren’t in the hospital
1:28:23.125,1:28:26.166
just really didn’t understand
what it was like to be there.
1:28:26.166,1:28:30.500
And so probably supporting each other
about how hard it was,
1:28:30.500,1:28:34.083
what an important thing to do. Right.
1:28:35.166,1:28:37.291
So lots of ways that you are
1:28:37.291,1:28:40.125
showing up with compassion
that really made a difference.
1:28:40.541,1:28:40.833
Yeah.
1:28:40.833,1:28:45.083
And similar probably for patients to write
that everybody was scared
1:28:45.083,1:28:47.583
and things were so uncertain.
1:28:48.583,1:28:49.958
Yeah, so comforting.
1:28:49.958,1:28:52.083
Patients. Yeah.
1:28:52.083,1:28:52.416
Okay.
1:28:52.416,1:28:56.125
So notice you actually have some options
1:28:56.125,1:28:59.500
here.
1:28:59.500,1:29:01.458
It was super frustrating
1:29:01.458,1:29:05.583
that you didn’t get the support you needed
from management, from the hospital
1:29:05.583,1:29:10.291
and understandably caused you pain
because you want to make things better.
1:29:10.375,1:29:14.500
You wanted people to have healthier lives
and you just noticed
1:29:15.208,1:29:18.458
there’s a lot of flexible ways
that you can express your values.
1:29:18.833,1:29:23.500
So we want a lot of different options
up here because we find ourselves
1:29:23.833,1:29:28.041
in contexts and external situations
that limit our options.
1:29:28.041,1:29:31.416
So resiliency on
this side is really having
1:29:31.833,1:29:35.000
quite a few ways
to show up towards what matters to you.
1:29:35.958,1:29:38.000
I want you to notice two Dr.
1:29:38.000,1:29:41.791
Dayna down here, these things
that matter to you are the very things
1:29:42.541,1:29:44.625
that are connected to your pain.
1:29:44.625,1:29:48.250
So looking at anger, frustration
helpless, hopeless
1:29:48.250,1:29:52.791
because you cared about patients
and your colleagues, memories of people
1:29:52.791,1:29:55.583
being harmed because you want them
to be healthy and feel better.
1:29:56.666,1:30:00.541
And this is not fair because you want
things to be fair for these people.
1:30:01.041,1:30:05.416
So your pain is directly connected
to these values
1:30:05.958,1:30:10.416
and then that way risk and resiliency
are two sides of the same coin.
1:30:10.958,1:30:13.333
We hurt because we care.
1:30:13.541,1:30:16.958
So when you look at this whole matrix,
what’s it like to?
1:30:16.958,1:30:19.500
Notice with kindness and curiosity?
1:30:19.500,1:30:19.833
Yeah, it’s
1:30:19.833,1:30:24.625
actually it’s pretty clarifying too,
to see it like written out all that way.
1:30:24.625,1:30:27.958
And I can see that I was getting stuck,
1:30:28.208,1:30:31.541
you know, in
just one way of trying to do things.
1:30:31.541,1:30:32.708
And that maybe there are
1:30:32.708,1:30:37.416
some other things that I could do
that are still important and helpful.
1:30:38.708,1:30:41.583
Yes. And
here’s what’s important to notice.
1:30:41.583,1:30:44.583
We we don’t get to get rid of the away
side or side.
1:30:45.291,1:30:49.000
The uncertainty
the pain of life is is there for good.
1:30:49.833,1:30:54.625
And yet we do get to focus on continuing
to move towards a meaningful life.
1:30:54.625,1:30:59.541
Even with that, even with the ways
that we’re managing that pain.
1:30:59.708,1:31:02.083
So today you noticed
1:31:02.708,1:31:05.291
different ways to move to the towards side
1:31:05.791,1:31:10.541
and how we are resilient
even in the face of difficult situations.
1:31:11.291,1:31:16.000
So that was an example of how you can use
the matrix to understand what’s going on
1:31:16.000,1:31:19.958
for us and to take a new perspective
on how we can move forward.
1:31:20.583,1:31:21.458
As clinicians.
1:31:21.458,1:31:22.541
We use this all the time
1:31:22.541,1:31:26.250
to help our clients and patients,
but we also use this in our everyday life.
1:31:26.541,1:31:30.625
Whenever I’m feeling confused
or stuck or uncertain about how to behave,
1:31:30.625,1:31:32.500
I will take out a matrix and fill it out
1:31:32.500,1:31:36.000
to figure out what’s important to me
and how can I express that?
1:31:36.375,1:31:39.291
We can really see
how risk and resiliency are
1:31:39.875,1:31:44.750
part of two sides of the same coin
that we can get stuck on the away
1:31:44.750,1:31:47.791
side is part of the risk,
and it’s a normal human response.
1:31:48.041,1:31:52.041
And resiliency is figuring out ways
to make towards moves even when it’s hard.
1:31:53.583,1:31:54.791
Yeah, the Matrix has
1:31:54.791,1:31:58.583
me really listen to my pain
and find my values within my pain.
1:31:59.250,1:32:02.791
So when I am feeling angry, what
1:32:03.875,1:32:07.916
feels wrong to me that I could take
valued actions on when I’m sad?
1:32:07.916,1:32:11.166
What can I
what can I mourn that matters to me?
1:32:11.791,1:32:15.958
And if I’m scared,
what can I protect that I care about?
1:32:16.541,1:32:18.708
If I’m guilty, what can I repair?
1:32:18.708,1:32:23.375
So my pain then informs my values
and my valued actions
1:32:23.708,1:32:26.875
instead of being something
I need to react to and fix.
1:32:27.833,1:32:31.041
So we always take the approach
that wellness
1:32:31.041,1:32:35.041
is a joint responsibility
between employees and employers.
1:32:35.041,1:32:39.875
So although we don’t have time in today’s
presentation, there is also a team matrix
1:32:39.875,1:32:43.583
or a pro-social matrix, which is about
how groups can work together
1:32:43.833,1:32:46.666
and find their shared purpose
or their values
1:32:46.666,1:32:49.833
and move towards or away
from that and understand that better.
1:32:50.125,1:32:54.916
And so we want to empower individuals
to do what they can to be.
1:32:54.916,1:32:58.416
Well, while we also recognize that systems
also need to change
1:32:58.416,1:33:06.708
to help the individuals
be well, incredible stuff.
1:33:06.708,1:33:09.291
Thank you so much to Dr.
1:33:09.416,1:33:10.958
Jaimie Lusk and Dr.
1:33:10.958,1:33:14.541
Dayna Lee-Baggley. And Dr.
1:33:14.541,1:33:19.541
Dayna is is joining us today,
along with Dr.
1:33:19.541,1:33:21.916
Suzette and Dr. Lorraine are back.
1:33:22.750,1:33:24.125
Thank you all so much.
1:33:25.500,1:33:27.541
You know,
talking about the problem is so important,
1:33:27.541,1:33:32.875
but providing the tools to address
those problems is crucial
1:33:33.125,1:33:37.000
if we’re going to change
personal and institutional behaviors.
1:33:37.000,1:33:40.250
And thank you, Doctor.
1:33:40.250,1:33:41.291
What was it like, Dr.
1:33:41.291,1:33:46.083
Dayna, to go through the Matrix yourself?
1:33:46.083,1:33:49.333
You gave so much of yourself,
and I don’t think that those answers
1:33:49.333,1:33:50.458
were made up.
1:33:50.458,1:33:53.541
Like I’m not thinking that. Yeah.
1:33:53.583,1:33:58.250
So I really do actually use the Matrix
all the time in my everyday life.
1:33:58.250,1:34:01.958
So going through the Matrix
was a really common thing for me,
1:34:02.250,1:34:05.166
but I think it really demonstrates
how we can do it.
1:34:05.166,1:34:09.166
We were really glad to have some real,
you know, lived experience to be able
1:34:09.166,1:34:12.416
to share with the audience
and how we could use the Matrix
1:34:12.416,1:34:13.625
with that lived experience.
1:34:13.625,1:34:19.250
And so I think it’s a great example
with them, you know, real data
1:34:19.250,1:34:22.958
as to how you can make use of it
to handle the experiences of
1:34:23.625,1:34:25.375
frontline workers during a pandemic.
1:34:25.375,1:34:26.958
And hospital workers in general
1:34:28.166,1:34:29.875
are sure.
1:34:29.875,1:34:33.000
I want to just remind folks that the Q&A
1:34:34.333,1:34:37.333
box is open to you if you have questions
1:34:37.333,1:34:40.000
for the university of Alberta team here,
1:34:41.250,1:34:44.750
I’m happy to,
1:34:44.750,1:34:47.875
you know, express those questions for you
right here.
1:34:48.625,1:34:51.458
I do wonder about this.
1:34:51.458,1:34:54.583
There is a question that came up
about the group and team Matrix
1:34:54.583,1:34:58.375
that you did mention and how that works
1:34:58.375,1:35:00.458
and how can you just
1:35:02.916,1:35:05.791
either anyone of you can
can you tell me just a little bit
1:35:05.791,1:35:09.041
about how the team Matrix
1:35:09.041,1:35:12.500
would be applied in health care settings?
1:35:12.500,1:35:14.708
It how it might work?
1:35:15.041,1:35:17.583
So we visited in a number
of our interventions
1:35:17.583,1:35:21.250
with health care workers
and it’s really four kind of group.
1:35:21.250,1:35:22.708
So it could be a unit,
1:35:22.708,1:35:26.375
it could be a department,
it could be two people working together.
1:35:26.708,1:35:31.125
And what it allows groups of people to do
is to focus the conversation on values,
1:35:31.125,1:35:35.208
which in the group setting
we refer to as shared purpose in groups.
1:35:35.208,1:35:38.166
We, you know, and in work settings,
there is a shared purpose
1:35:38.166,1:35:40.291
that people are there
to do something together.
1:35:40.750,1:35:44.500
And so it allows us to have conversations
about shared purpose
1:35:44.500,1:35:49.208
and values instead of again,
like right, wrong, but bad, true, false.
1:35:49.750,1:35:52.250
We used it in work conflict
1:35:52.250,1:35:56.083
resolution to again change the perspective
instead of like who’s right
1:35:56.083,1:35:59.500
and who’s wrong in terms of
what’s going to move us towards.
1:35:59.500,1:36:03.000
In a way we use it in our diversity,
equity and inclusion
1:36:03.000,1:36:06.333
training to help people change
their behavior in their everyday lives.
1:36:06.333,1:36:10.500
Again, becoming more aware of the biases
that show up and choosing behaviors
1:36:10.500,1:36:13.250
that’s more consistent,
their values around inclusion.
1:36:13.833,1:36:16.416
So there’s a number of ways
that you can make use of it,
1:36:16.416,1:36:18.458
and it’s a really versatile tool.
1:36:18.458,1:36:20.625
Again, it’s really meaningful to us.
1:36:20.916,1:36:24.333
In addition to empowering individuals
is to help change the systems.
1:36:24.333,1:36:30.000
We know that the systems are also
contributing to burnout, contributing
1:36:30.041,1:36:34.125
to moral injury, and so we don’t want to
just rely on the individual changing.
1:36:34.125,1:36:36.125
We also want to help the system change.
1:36:36.125,1:36:39.458
And so we’ve made use of that tool,
for example, in leadership training,
1:36:39.458,1:36:41.708
which is one way that you change
the system is by helping
1:36:41.708,1:36:46.083
leaders have better skills
to manage people and to make decisions.
1:36:46.291,1:36:51.583
And so there’s a number of ways
that we’ve made use of it in teams.
1:36:51.583,1:36:58.166
Oh, you’re on meet.
1:36:58.166,1:37:00.208
It’s like I’m brand new at this.
1:37:00.750,1:37:02.458
I’m really not.
1:37:02.458,1:37:04.500
Can you just tell me
how it’s been received then?
1:37:04.500,1:37:09.083
In those in those settings you say that
it’s been that The Matrix has been applied
1:37:09.083,1:37:11.375
to so many different
1:37:12.166,1:37:16.333
scenarios and, and groups
how has it been received?
1:37:16.333,1:37:21.833
Has has there been uptake in the
in the way I know that you and Dr.
1:37:21.833,1:37:25.000
Jaimie have used use it in your own lives.
1:37:25.000,1:37:26.583
Tell me a little bit more about the uptake
1:37:27.875,1:37:29.458
and how it’s received.
1:37:29.458,1:37:31.958
Yeah. So I think it’s been very favorable.
1:37:31.958,1:37:36.458
We did a study on burnout
during the pandemic and again
1:37:36.458,1:37:39.666
we decided that we
we got grant funding to look at
1:37:40.750,1:37:44.416
burnout in frontline workers and we chose
to do a leadership training of,
1:37:44.666,1:37:48.083
you know, an employee training to again,
try to address some system level problems.
1:37:48.083,1:37:52.041
And that was the structure
of all of the intervention
1:37:52.041,1:37:54.791
was using the matrix
to help change behaviors of leaders.
1:37:54.791,1:37:57.458
And so it’s been really,
really well-received.
1:37:57.708,1:38:01.291
One of the things the Matrix does
is actually create psychological safety.
1:38:01.291,1:38:03.125
And so that’s sort of been mentioned
1:38:03.125,1:38:07.083
in some of the earlier talks as well
about lacking psychological safety.
1:38:07.083,1:38:11.625
And it’s actually a tool that teams
can use that builds psychological safety
1:38:11.625,1:38:12.708
because it allows people
1:38:12.708,1:38:16.250
to have conversation
about difficult topics in a safer way.
1:38:16.541,1:38:17.916
So we don’t have to point out
1:38:17.916,1:38:21.458
like, well, you did this or you did that
or this was bad or you shouldn’t do that.
1:38:21.708,1:38:23.291
We can simply say kind of that
1:38:23.291,1:38:26.291
felt like a towards move for me
or that felt like an away move for me.
1:38:26.500,1:38:30.333
And sometimes, you know,
people are trying to do towards moves
1:38:30.333,1:38:34.791
and they’re interpreted as a way moves
and so it gives a team a language that you
1:38:34.791,1:38:39.458
that is really more compassionate and
more flexible and more curious and open
1:38:39.833,1:38:43.833
and doesn’t have to get into like,
right, wrong true, false, good, bad.
1:38:44.541,1:38:47.083
Right.
And it started one of those earworms.
1:38:47.083,1:38:50.250
You know, once you hear towards in a way
like it’s hard to forget it.
1:38:51.083,1:38:53.000
Absolutely. Absolutely.
1:38:54.541,1:38:55.791
Dr. Lorraine and Dr.
1:38:55.791,1:39:01.708
Suzette, have you been applying the matrix
to your lives?
1:39:01.708,1:39:03.541
Yes, absolutely.
1:39:03.541,1:39:04.750
As Dr.
1:39:04.750,1:39:08.458
Dayna just said, it’s amazing how familiar
this idea
1:39:08.500,1:39:11.583
towards in a way becomes
and is documented.
1:39:11.583,1:39:14.250
I think it’s a really nice way
to sort of ask yourself,
1:39:15.833,1:39:18.333
why am I doing this behavior right?
1:39:18.333,1:39:21.500
And what does it mean to me
that I am doing this behavior?
1:39:22.000,1:39:25.708
And so for me personally,
that has been a great way to clarify
1:39:25.708,1:39:29.000
why am I doing certain things
and really to be able to look and say,
1:39:29.000,1:39:30.250
is this towards
1:39:30.250,1:39:33.958
what I care about, as Suzette said,
is this something that’s meaningful to me?
1:39:34.166,1:39:36.875
Does it move me
in the way that I want to move in my life,
1:39:37.250,1:39:41.958
or is it really taking me away from that,
even if it’s a short term experience?
1:39:41.958,1:39:45.791
So it really has helped me
to to really clarify
1:39:45.833,1:39:50.166
that meaning and purpose in my life
in really small ways, really tiny things
1:39:50.166,1:39:54.250
that I’ll ask myself, like, you know, work
decisions or personal decisions.
1:39:54.250,1:39:56.791
So yeah, definitely I’ve used it
1:39:57.833,1:39:58.250
and I
1:39:58.250,1:40:01.125
would just do, I would just echo
that if I could.
1:40:01.375,1:40:03.041
Yeah, yeah.
1:40:03.041,1:40:04.875
Of just being empowering.
1:40:04.875,1:40:08.750
So a tool that I use as well in terms
of making those choices.
1:40:08.750,1:40:11.166
So looking, do I go this way
or do I go that way?
1:40:11.166,1:40:13.125
It’s, it’s within my control.
1:40:13.125,1:40:16.750
And so giving people reminding people,
reminding me of my choice.
1:40:16.750,1:40:19.208
And so I find the tool very empowering.
1:40:19.208,1:40:23.458
Also, it challenges me to be more aware,
1:40:23.583,1:40:29.041
more self aware, and more collectively
aware of what choices we’re taking.
1:40:29.041,1:40:32.041
I choose to look at something,
what other options I have.
1:40:32.041,1:40:36.500
So for me it’s an awareness tool as well
as a choice tool and a team building.
1:40:36.500,1:40:37.083
And it’s Dr.
1:40:37.083,1:40:41.250
Dayna mentioned as, well,
a way for people to have a safe way
1:40:41.583,1:40:45.416
to not look at blacks and whites
or or blaming or otherwise,
1:40:45.416,1:40:49.416
but to really have an open mind about
seeing things in a broader perspective.
1:40:49.416,1:40:52.041
So empowering choice breadth
1:40:52.750,1:40:57.083
about me and about weight
and really keeping that focus on two sides
1:40:57.083,1:40:59.125
of the same coin
and looking at where those
1:40:59.500,1:41:02.416
where those pains are,
also the things that truly matter.
1:41:02.708,1:41:05.791
And how if I root into those,
I can be more resilient
1:41:06.416,1:41:08.666
in even the most difficult
of circumstance says.
1:41:09.125,1:41:11.750
So I think for me it’s
something it’s a lens through which
1:41:11.750,1:41:16.125
I look all the time
to be able to make the choices that I do.
1:41:16.125,1:41:20.291
So rather than a tool for me
it’s a way of life and a lens through
1:41:20.291,1:41:23.375
which I look at every moment
of every life about Do
1:41:23.375,1:41:26.791
I choose to move this way or that way? I’m
1:41:27.750,1:41:29.333
amazing.
1:41:29.375,1:41:34.250
I feel like The Matrix is something
that I’m going to take back to all of,
1:41:34.458,1:41:38.625
you know, my own teammates and my own life
1:41:38.625,1:41:42.250
and put it on the fridge
and all of you here where
1:41:43.500,1:41:46.041
it really is.
1:41:46.041,1:41:48.750
You know,
one thing that I find really fascinating
1:41:48.750,1:41:51.958
is the idea that The Matrix helps
1:41:51.958,1:41:54.750
to clarify your values
1:41:55.125,1:41:59.250
and and how values link with resilience.
1:41:59.250,1:41:59.791
So I’m wondering,
1:41:59.791,1:42:02.958
you just unpack that just again,
just a little bit more so that we can be
1:42:03.375,1:42:06.750
left with a clarity
in, in that how the values
1:42:09.250,1:42:11.416
are linked with resilience
1:42:11.416,1:42:16.416
and then how you can get to that
through the matrix DOT data.
1:42:16.416,1:42:19.208
So one of the great parts about the Matrix
is it is an evidence
1:42:19.208,1:42:23.000
based tool and it’s built on, you know, a
well-supported intervention known
1:42:23.000,1:42:26.208
as acceptance and commitment therapy
that’s been shown to address
1:42:26.208,1:42:29.208
that number of conditions
from things like depression and anxiety.
1:42:29.708,1:42:32.083
Our team used it for moral injury,
1:42:32.541,1:42:35.250
but also even things
like OCD and psychosis.
1:42:35.541,1:42:38.250
And then things like procrastination
and parenting.
1:42:38.500,1:42:41.916
And so it’s a very versatile therapy,
but well-established
1:42:42.291,1:42:43.416
that we know that it works.
1:42:43.416,1:42:46.166
And so values
as part of that model of therapy
1:42:46.416,1:42:50.125
and values has a very kind of specific
meaning in, in the therapy
1:42:50.125,1:42:53.250
is that it’s about
how you want to show up as a person.
1:42:53.583,1:42:56.291
And that’s really important
because it’s not sort of like,
1:42:56.291,1:42:58.375
what do I want to get out of life?
1:42:58.375,1:43:00.458
But it’s like,
what do I want to contribute to life?
1:43:00.458,1:43:02.041
How do I want to care about people?
1:43:02.041,1:43:03.750
How do I want to show up?
1:43:03.750,1:43:05.708
And that’s a much different thing
to think about
1:43:05.708,1:43:09.083
because then it’s about your own behavior
and you have much more control over that
1:43:09.333,1:43:12.875
than the environment or,
you know, the way the world is responding.
1:43:13.500,1:43:16.166
And so, you know, for example, sometimes,
1:43:16.166,1:43:19.291
you know, there was people who would say
freedom is a value.
1:43:19.291,1:43:22.333
And the question was, well,
what would you do with more freedom?
1:43:22.458,1:43:22.791
Right?
1:43:22.791,1:43:25.458
Because the values part is
how would you show up
1:43:25.791,1:43:28.916
if that’s important to you, how would
what would you do more of or less of
1:43:29.125,1:43:29.916
if you have that?
1:43:29.916,1:43:32.291
That’s
how we kind of talk about the values.
1:43:32.916,1:43:35.416
And so there’s a, you know, Dr.
1:43:35.416,1:43:37.750
Jaimie did a great example of that.
1:43:37.750,1:43:40.791
There’s this expression about where
there is pain, you’ll find your values.
1:43:40.958,1:43:43.750
And so that’s it’s
the two sides of the same coin
1:43:44.000,1:43:48.333
that when something is really painful,
it also tells you what’s important to you.
1:43:48.333,1:43:50.250
And it can give you clues
1:43:50.250,1:43:53.250
about, you know, what matters to you
and how you want to show up.
1:43:53.500,1:43:57.333
And then there’s the secret sauce is
then we want to find flexible
1:43:57.333,1:43:59.083
ways of expressing that. We often get
1:44:00.083,1:44:01.833
into very narrow definitions
1:44:01.833,1:44:05.166
of like, this is how I have to show up
to express value.
1:44:05.166,1:44:08.666
But we’re trying to find lots
of different ways to express our values.
1:44:08.666,1:44:12.541
And that, I think, is really important
in this world that this like
1:44:12.750,1:44:15.666
post-pandemic world
that is way more uncertain.
1:44:15.666,1:44:20.791
And there is a lot of things that are less
predictable than they were beforehand.
1:44:20.791,1:44:23.625
And so having that
psychological flexibility to show up
1:44:23.875,1:44:26.416
in a variety of different ways
to express your values
1:44:27.000,1:44:30.500
then gives us a lot of ways
to move forward in a meaningful way.
1:44:31.708,1:44:36.250
Yes. Thank you very much for this.
1:44:36.250,1:44:38.416
This has been
1:44:38.791,1:44:40.416
such a
1:44:41.750,1:44:43.958
paradigm shifting in your head.
1:44:43.958,1:44:45.958
You know that these shifts, something
1:44:46.958,1:44:51.250
this just this
the matrix is is really quite fascinating.
1:44:51.250,1:44:52.500
If anyone
1:44:52.500,1:44:56.916
wants to take a look at the template,
you can look at the chart right now.
1:44:57.125,1:44:58.958
There’s a French version.
1:44:58.958,1:45:01.291
It’s also in other languages.
1:45:01.291,1:45:03.750
There’s an English version
here in the chat.
1:45:04.416,1:45:07.041
You’ll see that
and you can just copy and paste that.
1:45:07.791,1:45:12.750
There’s also a question here about a link
to, the group and Team Matrix,
1:45:13.125,1:45:16.625
which we I’m sure
that we can provide as well.
1:45:17.250,1:45:18.625
But I want to thank Dr.
1:45:18.625,1:45:21.583
Suzette Brémault-Phillips, Dr.
1:45:21.583,1:45:23.833
Lorraine Smith-MacDonald, Dr.
1:45:24.125,1:45:28.000
Dayna Lee-Baggley and Dr.
1:45:28.000,1:45:30.250
Jaimie Lusk, who is not with us right.
1:45:30.250,1:45:31.791
But this has been fascinating.
1:45:31.791,1:45:37.583
Thank you so very much
for being part of the symposium day.
1:45:37.583,1:45:38.833
Thank you so much.
1:45:38.833,1:45:41.500
Thanks for the opportunity. Thanks, Dayna.
1:45:41.500,1:45:45.458
Thanks, Lorraine. So
1:45:47.333,1:45:50.291
the University of Alberta
doing some really incredible things.
1:45:50.291,1:45:53.166
I love it.
1:45:53.166,1:45:56.000
Now, if you can believe it, we have come
1:45:56.458,1:45:59.416
to the end of symposium today.
1:45:59.708,1:46:01.000
I want to
1:46:02.500,1:46:05.250
invite again actually, I want to
1:46:06.541,1:46:10.791
thank everyone
who has been a part of this today
1:46:10.791,1:46:13.708
for taking the time and being so generous
1:46:14.708,1:46:17.625
and and open.
1:46:17.625,1:46:20.333
Those health care professionals
and the audience
1:46:20.625,1:46:24.291
who took the time to take part
and be in the symposium.
1:46:24.583,1:46:27.833
I know those that were that were speaking.
1:46:27.833,1:46:31.750
It takes a great deal of courage
to share your experience.
1:46:31.750,1:46:36.916
And then those in the research fields
that marry all that experience
1:46:36.916,1:46:40.833
with the depth and breadth of research
and offer up tools like.
1:46:40.833,1:46:42.166
The Matrix
1:46:43.166,1:46:45.541
I know that the work that you’re doing is
1:46:45.541,1:46:49.750
is just so difficult,
but so important, though.
1:46:49.750,1:46:50.875
Thank you.
1:46:50.875,1:46:53.250
I now I’d like to welcome back Dr.
1:46:53.250,1:46:56.833
Margaret MacKinnon for a short debrief on
1:46:57.708,1:47:00.791
on everything that we’ve heard today.
1:47:00.791,1:47:03.583
We’re just pouring in with
thanks for all of the
1:47:04.083,1:47:07.583
all of the
the panelists and for the symposium.
1:47:08.708,1:47:09.833
Dr. MacKinnon.
1:47:09.833,1:47:11.166
Margaret,
1:47:12.000,1:47:13.583
this has just been great.
1:47:13.583,1:47:18.458
I mean, can you I know that you’re
intimately familiar with the research
1:47:18.458,1:47:23.125
and the tools that were presented today,
and you’ve heard so many stories.
1:47:23.458,1:47:26.500
What has today’s symposium taught you
1:47:26.708,1:47:29.375
about risk and resilience
1:47:30.708,1:47:31.541
So much?
1:47:31.541,1:47:36.125
And I just want to echo your words and
thanking everyone who contributed today.
1:47:36.500,1:47:39.375
It is not easy to tell these stories.
1:47:39.375,1:47:41.541
It’s hard to listen to them.
1:47:41.541,1:47:44.041
But I think what I learned
and was reminded of again today is
1:47:44.041,1:47:46.208
that we’re not alone in this.
1:47:47.125,1:47:50.166
You know, in speaking to health
care workers often hear people say it’s
1:47:50.416,1:47:52.000
I feel so alone.
1:47:52.000,1:47:53.583
I don’t think other people necessarily
1:47:53.583,1:47:57.750
are having the same experiences
because we are having the same reactions.
1:47:57.750,1:48:01.666
And I think what reminded here
today, it’s a community that we share
1:48:02.000,1:48:06.583
and the work that we have to do together,
and that includes organizations,
1:48:06.875,1:48:10.875
individuals, members of government,
policymakers.
1:48:11.250,1:48:13.958
We’re in this together
to support one another.
1:48:14.291,1:48:17.375
And just being reminded
and knowing of these stories,
1:48:17.708,1:48:22.416
knowing the tools that can help us
and working together towards a common
1:48:22.416,1:48:25.416
purpose of supporting and strengthening
1:48:25.791,1:48:28.833
our health care worker community.
1:48:28.833,1:48:29.750
Absolutely.
1:48:31.291,1:48:34.666
If you want, wanted to have
1:48:35.791,1:48:38.250
folks in the audience walk away with.
1:48:38.250,1:48:41.541
You know, just one thing today.
1:48:41.875,1:48:45.458
I know there’s many that we spoke about,
and I know this is putting pressure on you
1:48:45.458,1:48:48.875
because maybe I didn’t tell you
that I was going to ask this question,
1:48:48.875,1:48:54.208
but what would that what would you want
folks to walk away from with today?
1:48:54.666,1:48:56.458
Yeah, I know.
1:48:57.000,1:48:59.166
I’ve worked
as a clinical psychologist in the past,
1:48:59.166,1:49:00.750
and I think
one of the most difficult things
1:49:00.750,1:49:04.750
when we face trauma is often
to reach out to others for support.
1:49:05.583,1:49:08.041
You know, I’ve worked with patients
where even making a phone call
1:49:08.416,1:49:11.166
is painful, it’s difficult, it’s hard.
1:49:11.500,1:49:13.375
And I think
certainly when we’re in situations
1:49:13.375,1:49:17.125
like this, we do have a tendency often
to turn inwards and.
1:49:17.125,1:49:21.000
What I want to encourage
people to do is turn to one another.
1:49:21.666,1:49:23.333
We’re here to support each other.
1:49:23.333,1:49:28.541
We have each other’s backs, are part of
a community that’s of service who serve.
1:49:28.875,1:49:32.208
And we want to thank you again,
all of you, for your service.
1:49:33.291,1:49:35.333
Thank you so much.
1:49:35.333,1:49:37.708
Now you’re going to see up on the screen
1:49:37.708,1:49:39.750
to follow us here.
1:49:40.958,1:49:43.708
Then, if you’d like to take a look
at the research,
1:49:43.708,1:49:45.875
there’s the website, social media.
1:49:46.208,1:49:47.416
It’s all up.
1:49:47.416,1:49:50.708
It’ll come up on the screen
and you can follow along
1:49:51.750,1:49:56.333
with the resources bbc.co.uk and to a FAQ
1:49:56.625,1:49:59.708
and all of the partners and sponsors.
1:49:59.708,1:50:03.750
Thank you to everyone
who has taken the time to be here today.
1:50:03.750,1:50:08.250
We hope that you are leaving here
with helpful takeaways.
1:50:09.541,1:50:13.000
If you want to leave
just one word in the chat
1:50:13.000,1:50:17.166
about how you are feeling about this
session, please do.
1:50:18.166,1:50:23.041
It’s always nice to see
how folks are feeling, but as I said,
1:50:23.375,1:50:27.666
please take a look at the resources
that here and you can go back
1:50:28.625,1:50:30.833
to this video at a later date.
1:50:31.291,1:50:33.125
Thank you again for joining.
1:50:33.125,1:50:36.208
Have a wonderful day and
1:50:37.208,1:50:51.833
thank you.