Symposium 3: Navigating the fog
The COVID-19 pandemic has resulted in unprecedented and often devastating new circumstances for healthcare providers (HCPs), leading to an increased need for mental health prevention and early interventions efforts to support this critical workforce.
This two-hour event features:
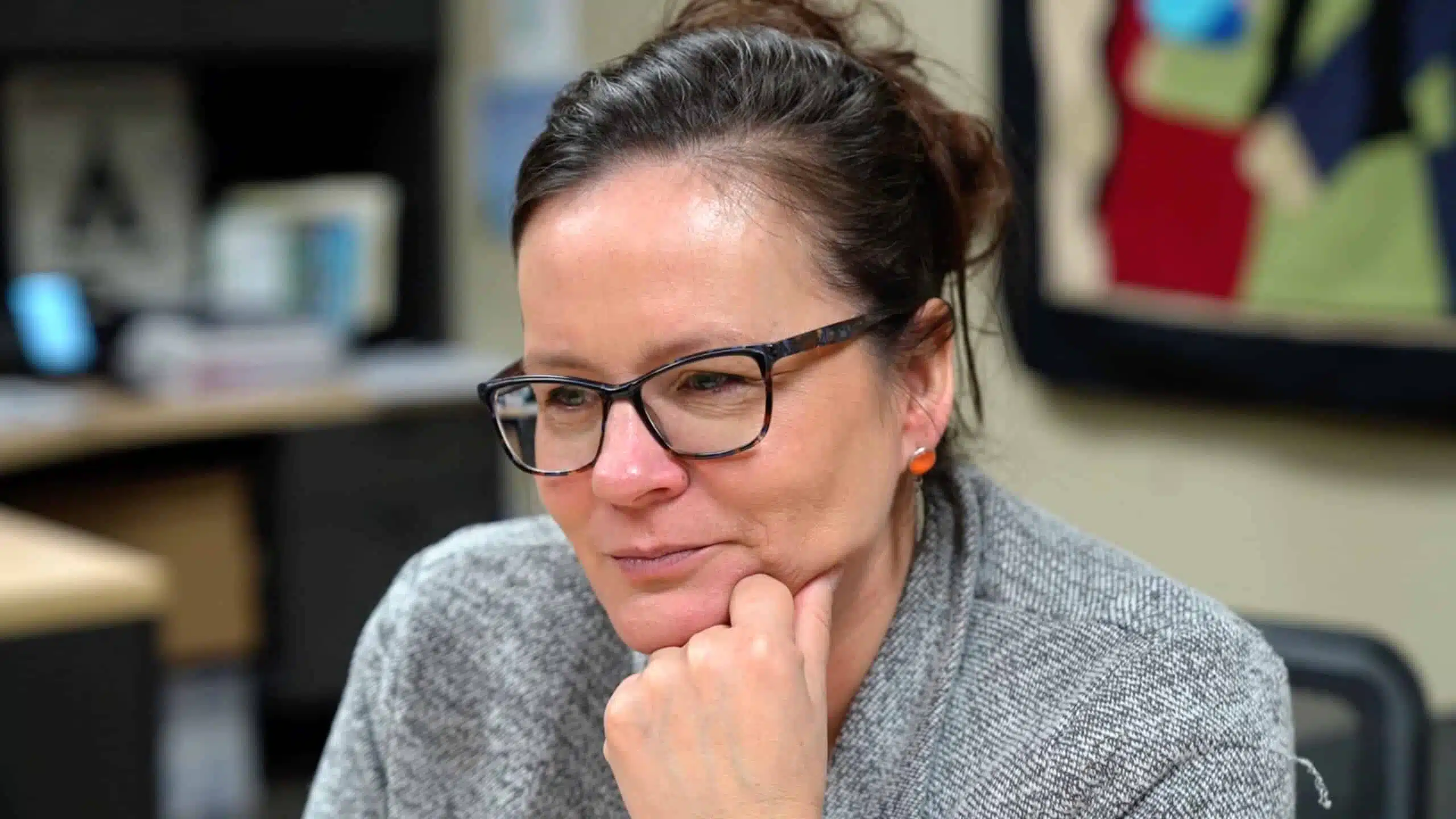
- Live moderated chats featuring Dr. Margaret McKinnon, principal investigator of Healthcare Salute, and healthcare leaders with lived experience of the COVID-19 pandemic
- A research presentation about leadership during the pandemic by Dr. Aneesh Joseph of the Trauma & Recovery Research Unit at McMaster University
- A panel discussion to share updates from our researchers and invited guests on what the emerging research is showing
- Audience Q&A sessions follow our discussions

CONTENT WARNING
During this event, we discuss examples of moral distress, moral injury, and other challenges in the work life and home life of healthcare providers during the COVID-19 pandemic. Some moments may be disturbing for you. It’s fine if you wish to stop watching at any point.
If you require wellness support, we encourage you to follow this link.
Transcript
Hello and I guess this is good afternoon or maybe good morning. My
name is Garvia Bailey and I will be your moderator for today’s symposium. Welcome,
on behalf of the McKinnon Trauma and Recovery Lab’s PHAC project Healthcare
Salute. This symposium is called “Navigating the fog: The role of
healthcare leaders in supporting provider mental health during the COVID-19
pandemic.” I am a journalist by trade, a storyteller by nature, and every now and
again, I have the great fortune to be asked to
moderate an event like this one. I consider this legacy work. These deep
conversations, the research in institutions like McMaster, set the
agenda for the actions we should be taking and the conversations we should
all be having before, during, and deep into the long tail of an international
crisis like we are facing with COVID. So, I want to thank you for being here. I
would like to acknowledge the land that we’re on right now. My family came here
from Jamaica in the 1970s, and we continue to be ever so
fortunate and grateful to have come to this
country and be on this land and this territory as immigrants and settlers. I
live and work on land that we recognize as the traditional territories of the
Haudenosaunee and Anishinaabe Nations and recognize and act on the responsibility
that comes with that. I’d also like to acknowledge the land on which McMaster
University is located, which is the traditional territory of the Haudenosaunee and
Anishinaabe Nations and within the lands protected by the Dish with One Spoon
Wampum Belt. The wampum uses the symbolism of a dish to represent the
territory and one spoon to represent that the people are to share the
resources of the land and only take what they need. Further to that, the Truth
and Reconciliation Commission’s 94 Calls to Action reaffirm that the
treaties with Indigenous peoples must be lawfully honoured. We are all treaty
peoples and are responsible for honouring and upholding those
agreements. Again welcome to this symposium. Now over the past close to
four years, we have heard much about the strain on the healthcare system and on
healthcare providers due to the pandemic. But those providers are not
rudderless; they are steered by leaders and it’s impossible to paint a complete
picture or look to solutions without looking closely at
leadership and how leaders can better support their teams. Today we will hear
from researchers from across the country doing the work to quantify and pinpoint
the pressure points for those working in healthcare and offer up valuable
solutions and best practices. We will hear personal stories, dig into the
challenges and concerns from the perspective of leaders, and healthcare
workers. Today we have two leaders who were in the front lines during the
height of the pandemic. John Yip, who is the CEO of SE Health, and Dr. Heather
Morrison, PEI’s Chief Medical Officer of Health. So, today is about sharing
knowledge and experiences and marrying that with deep research, which
hopefully leads to a cultural shift. Learning and adapting through crisis is
a true mark of leadership. If you’re a healthcare worker and/or occupy a
leadership position and you’re watching right now, we truly can’t thank you
enough for your service. So, some of what you might hear
today might be difficult to process. There will be links to wellness supports,
they’re linked here in this video but they will be in the chat as well,
so take a look at that if you feel like you just need a break. Thank you
to the Public Health Agency of Canada and all of our partners for their
commitment and support. This symposium is being recorded as part of the broader
research project, so you will have the opportunity to look back at this
symposium if you miss anything. There is an open chat function for this virtual
event. Please be respectful in your interactions and try and keep the chat
on topic, but it is open there for everyone to use. You know, maybe right now
just drop in the chat where you’re coming from where you’re at right now at
geographically, not spiritually, we don’t have to get into
all of that right now, but if you just let us know where you are, by dropping
that in the chat, that will be great! That’s where we’ll be interacting. We’ll
also interact in the Q&A. So, if you scroll on to your Zoom you’ll see
something called Q&A along the bottom. It’s to the right of the record button.
You can drop questions into the Q&A because there will be question and
answer periods after each session. And the chat is going to be
updated throughout the symposium by Sangita. Thank you so much Sangita for
doing that. Ancaster, hello! The Regina campus, good morning! Hello from Sudbury!
Lots of folks tuning in, I love it! And we have two sessions I should tell
you about today. One in the morning. We’re going to take a short break at about 12.
We have two sessions in the morning and then one in the afternoon so,
we’re going to take a break at 12 and then we’re going to come back after that,
so if you want to take a break then, that’s great. Hello Calgary, and hello
Winnipeg! Okay now, with leadership at the very top of mind, I’d like to now welcome
Dr. Margaret McKinnon, the team lead on this project. Hello, and good
morning Margaret. Wonderful to see you! It’s wonderful to see you, my friend! I
would say and you know I would be I think really remiss if I didn’t start by
thanking Media Girlfriends for their many, many contributions to this project
Garvia, Hannah Sung, and their teams have traveled across Canada, conducting
interviews with healthcare leaders, front line healthcare workers, along with
public safety personnel, to really tell the stories of those individuals who
faced the challenges of the pandemic head-on — who served at the front line as
leaders, on our hospital floors, in ambulances, and fire trucks, and police
cruisers throughout the pandemic. And Garvia and Hannah have really worked so hard to
tell the stories and I just want to thank you Garvia for everything that
you’ve done and Hannah. I also want to thank our production team, Make Things Well,
who has really been an incredible partner in this project, who created our
website, and has supported us throughout. I just wanted to acknowledge that in
this symposium series because we haven’t done that before, and I really did want
to do that. I want to also thank John Yip and Dr. Heather Morrison for being here
today. We so appreciate you being here. I want to also say that you know, I had
the honour and the privilege of serving on the front lines during the pandemic,
to provide mental health supports, and I spent time in the COVID-19 units, on
medical floors, supporting staff. But I also spent time with the senior
leadership teams, in the boardroom — I’m on a hospital board and also seeing the
challenges that leaders faced and I think at
times, it was difficult for people to know and appreciate what leaders also
experienced. I have been in rooms full of tears, because so many hard
decisions needed to be made. Often times, leaders were seen as the face of
something that they really had no control over. Decisions were often
changing in the moment. I am an academic leader and I know we would make
decisions and within seconds they would change, so I just want to also really
thank Dr. Morrison, John Yip for being here. But also to say thank you to all
of Canada’s healthcare leaders. You also made many services and many sacrifices
as did your families, and we just want to thank you for that. I also want to
quote something that John said during a video interview that was conducted
with him earlier that’s posted on our Healthcare Salute website. And John
said, you know I would never ask anyone to do something I wouldn’t do myself. And
I think that is really the marker of service among leaders. They also
went in, they served. Their families made many, many sacrifices. Often they weren’t
able to go home at night, they stayed there. I can recall being on a
COVID-19 unit for 36 hours, the majority of this in the storage
closet because it was the only time when people had a chance to take a break and
receive mental health support. And leaders were in the same position, so I
just want to acknowledge that it’s really, really important to acknowledge
your service and your sacrifice, as well. So, I’m going to now introduce Aneesh
Joseph. Dr. Aneesh Joseph. Aneesh Joseph is a member of our Trauma and Recovery
Lab here at McMaster. He received his PhD in Social Policy from Southampton
University, and he joined us recently in our group to conduct research and
also to provide real leadership around knowledge translation.
So bringing that research to Canadians trying to shape and influence
policy and healthcare practice through that work. Aneesh has spent much time also
working as an addictions counsellor as well. So in addition to his research
training, he’s also been on the front line. I really just want to thank
Aneesh most warmly for the work that he’s been doing. And all of the Healthcare
Salute team who have really been supporting this project. I think it’s an
important time to acknowledge everyone’s contributions and I really want to do
that. So, we’ll turn it over now to Dr. Joseph.
Thank you Garvia and Margaret. Hi, all. Thank you for joining us
today. I am happy to present the findings of our research on the role of
healthcare leaders in supporting provider mental health during the COVID-19
pandemic. At the outset, I would like to thank the team at the Trauma and Recovery
Research Unit at McMaster University under Margaret McKinnon, and all the
healthcare workers who participated in this
project. Since February 2021, a dedicated team at the lab have been working with
healthcare workers across Canada to research, analyze, and document the impact
of the pandemic on the mental health and well-being of the healthcare workers and
generate helpful tools and interventions to support
them. The findings can be accessed on our Healthcare Salute
website. These extensive research prompted us to look at the
organizational culture within the healthcare sector and look for areas and
elements that need to change for creating a better work environment that
supports the healthcare workers’ mental health and
well-being. The concept organizational culture
represents loosely how things are done here and how that affects the way
members think, feel, and behave. So cultural change will mean
moving from current state to a preferred state of how things are done
here. This presentation discusses some of the key elements of the current state of
organization culture and also will present recommendations that came from
the data to support how we envision a culture change within healthcare
organizations. With this intention, we surveyed and conducted semi-structured
interviews with healthcare workers from front line, middle management, and
leadership. The data have been thematically analyzed and will be
presented today. These are the demographic
information — age, provinces, and professions of the 24
healthcare workers who we interviewed for the
survey for the study. We used Organizational Culture
Assessment Instrument to understand and gauge how the members are thinking about
changes within the organization. OCAI scale is based on
comparing values framework and looks at four modes of culture within the
organization and seeks to understand the kind and direction of change they wanted
to happen within their
organization. Clan, adhocracy, and hierarchy and
market are four different segments within this
framework. Preliminary analysis show that there is a strong desire to move towards
clan. That represents collaboration, connection, trust, communication, and a
reasonable aspiration to incorporate. Adhocracy, which represents
innovation, cutting edge services, and growth. It is important to note that the
data shows an equally strong desire to move away from the current market
orientation and hierarchy in the organizational
culture. The qualitative data expounds the intensity and depth of this need and
aspiration for organizational culture change. We will be discussing the major
themes and sub-themes that emerged from the data, and we’ll be presenting them
as themes and
recommendations. While COVID-19 challenged everyone in the organization
in different ways, the healthcare workers acknowledge and appreciate the work that
the leadership and management did to steer through the difficulties of
pandemic. They also unpacked some of their concerns regarding the way current
organizational culture is constructed. Three major themes emerged
from the data that can be considered as challenging aspects of current culture:
widening disconnect, mismatch between words and actions, and misalignment of
priorities. Theme one: widening disconnect between leadership and front line.
Disconnect is delineated in words and phrases such as “distrust,” “invisible,” and
“unavailable,” “lack of presence,” “lack of transparency,” and “lack of understanding,”
“unilateral decision-making,” “hierarchy,” “feeling done to,” or “treated as a
pawn.” This disconnect was pronounced in the way decisions were made within the
organization.
There are considerable aspirations for engaging leadership that is present,
visible, and
accessible. Theme two: Mismatch between words and
actions. Words without actions were perceived as superficial, disingenuous, and
lip service. Especially when it comes to
supporting the mental health of the staff, these mismatch between words and
actions were considered to be eroding the trust within the
leadership. Fear of retaliation has been identified as a strong deterrent that
prevents staff from being open and from voicing their perspectives, concerns, and
genuine
feedback. That contributes to how they experience the
organization as a place where their mental health is not
supported. Theme three: Misalignment of priorities. There’s a perception that the
staff and leadership have divided priorities. While the staff — while the
organization wanted to be run like a business, the staff wants to prioritize
patient care and self-care. This division, this divided
priorities, keep them focusing on different aspects within the
organization and that focuses their energy in caring for different areas of
the organization and its
culture. “Being in a rudderless ship” suggests the experience of lack of direction,
initiative, and collaborative leadership. This has been an experience
of — especially when people came out of the
pandemic — they wanted strong direction to move everything forward from what has
been going through, and staff experienced a lack of leadership
initiatives in many aspects of organizational
culture. Some of the recommendations for moving towards a desired organizational
culture are as follows. The first recommendation is
rebuilding trust and fostering connections. The organizations need to
initiate processes and procedures that can rebuild trust and enhance connection
within the
organization. Rebuilding trust and fostering connection can help the
front line staff to feel heard, listened to, supported, and provide them with a
sense of belonging to the organization and its
work. Second recommendation is matching words with
actions. The organization needs to devise ways and
take — ways to take accountability for matching their words and actions and
also create ways to communicate those with the staff. The organization needs to
create mechanisms for ensuring that the values, policies, promises that it claims
to stand for are adhered to in the everyday dynamics of the work
environment. The third recommendation is prioritizing wellness,
safety, and mental health of the
staff. Following through critical incident debriefing, promoting self-care
for the staff, facilitating mental health support
(preferably onsite), and providing systemic support, such as manageable workload,
proper staffing, and higher allocation of funds for mental health in the benefit
and compensation package, can all help to embed these changes within
organization. When we really take these changes seriously and work towards
making it happen and making it embed within the organizational culture, that
will definitely lead to a trauma-informed organizational culture and work
environment, and towards trauma-informed
leadership. Thank you so much! With this, I conclude my presentation. I will now turn
it back to the
moderator. Thank you so very much, Dr. Aneesh Joseph. That was
wonderful, and really, some words that are sticking out: present, visible,
accessible. I feel like that presentation does an excellent job of
providing context and conversational fodder for the discussions that we’re
going to have today, and the discussion that we’re about to have right now with
two healthcare leaders. Now I should preface all of this by saying that this
is not putting these leaders on the hot seat. They’re not… this is not a session
that is meant to put their their feet to the fire. Because I’ve
spoken to both of these leaders at length and I know that they provide
the kind of leadership that the models that Dr. Joseph
put out just now — they very much adhere to this and I think it’s just
talking about their experiences being on the front lines during the pandemic.
John Yip is currently the CEO of SE Health. During the height of the pandemic,
John was the CEO of Kensington Health, a community not for-profit healthcare
provider in downtown Toronto. They provide community-based long-term
care, hospice, and ambulatory programs. Thank you for being here, John. And Dr.
Heather Morrison is the Chief Medical Officer of Health for Prince Edward
Island. Dr. Morrison also worked as an emergency room physician right up to the
beginning of COVID, so her experience spans not just being on the floor, but
being one of those leaders that a whole province was looking towards for help.
And I should add that the province itself loves Dr. Morrison, they really do!
They named a chicken after her, so — I don’t know who else can say that, but Dr.
Morrison can! Thank you both for being here. I want to start with a
question for both of you about Dr. Joseph’s presentation. Was there anything
in that that stood out or surprised you to learn any of this? I’ll start with
you, Dr.
Morrison. Good morning, good afternoon. It’s quite — it’s a
pleasure to be here. I’m in Charlottetown, Prince Edward Island, and so it’s nice to
see from the chat people from different parts of this wonderful
country. I think, you know, when I hear Dr. Joseph speaking,
I think the COVID pandemic highlighted and brought to the fore many issues that were
already there before and they highlighted them. So you know, we
probably did not have the best supportive environment for mental
health of our healthcare workers before COVID. And after COVID, we need it
more than ever. And so, it really wasn’t that it surprised me but I
think, it emphasized the fact that along with many other parts or things that
happened during COVID, it really got highlighted. Absolutely! For you,
John, was there something that that jumped out about Dr. Joseph’s
presentation? Well I wish I had a chicken named
after me! I think there’s a pig somewhere running around Ontario named
after me. I am based in Toronto. Thanks for inviting me to this session. I think
it’s critically important that we talk about these things. And I quite
enjoyed listening to the snippet, the video there of Dr. Joseph. And I agree with
Dr. Morrison’s comment — you can almost hear and read that paper
pretending that COVID never happened and that those findings would be exactly the
same findings pre-COVID and it would be just buried and no one would really pay
attention to it. If there’s any good that came out of COVID — there
are a couple good things, despite the tragedies
involved — is that the plight of our front line staff, the mental health and
well-being of our front line has been put to the forefront. And even now, dare I say
post-pandemic, it is still a major, major issue. And the pandemic did shine a
light on these issues that pre-existed and continue to exist right across
the country for our front line healthcare workers. Yeah. You know I had, as
we’ve mentioned, I had the pleasure of speaking to both of you in person
over the course of this summer and spent, you know, probably too many hours
sitting in front of you asking you some very pointed questions. And one of the
questions that — you know, you both talked about moments in which you
realized that there was a shift in what was happening. That this
pandemic was something that was unique, and that perhaps the way that you
were approaching leadership might have to shift slightly. Can you tell me about
what was happening? Can you paint the picture of when you realized that
this was something that would require something maybe that you hadn’t had
to, kind of, like, dig into post- COVID? I’ll start with you Dr.
Morrison. Well, I mean, in our experience here in PEI, I will preface it by
saying, it was different maybe in our province, compared to some of the other
provinces. And I think there were a few things.
One: how we managed when we realized how long this could last. I
think that was a big key thing — this was not going to be over in eight weeks,
like a SARS kind of journey. It was going to be much longer. So how we
we were going to get through this, and looking further ahead.
We — I said this at different times, so it may not have been at a
certain point, but we knew early on that we would not
always make the right decision. But we — and looking back, we knew that we would
make mistakes. But we knew we had to make the best decisions with the information
we had at that time. And make them for the right reasons! And if we were doing
that, that would help us going
forward. For us, in PEI, when Omicron came, almost two years
after the pandemic started, that was a huge shift for us. Because up until —
for almost two years, we did not have a death. We had hardly any hospitalizations.
We did not have a long-term care outbreak. But with Omicron, how we managed
had to shift, and we also had to lead differently to the public because
they weren’t used to seeing COVID. We had to
adjust with government, with our partners, and with the team here in
the office. So, that was probably one of the biggest times of
changing — knowing we had to change to learn how to live with, you know, we
heard often “have to live with COVID,” and for us that was really when Omicron came.
But it was like, the worst of the pandemic for us here, came at least when
we had vaccines and some of our processes and
PPE in place. I mean, those were some key points.
Yeah, for sure. John, for you, I know that there was a time in which you
spoke to your staff at Kensington Health at the time, and
said that “We have to do things differently.” Can you just
paint that picture — what was happening during that time, when
you realized that this was something unique, and would require some different
skills from you? Yeah, sure. Just to give people
context, Kensington Health has a 350-bed long-term care home on its site. It’s one
of the largest homes in downtown Toronto, and well sought after — the
waiting list is five years long. So, a lot of demand for the home, and I think
mainly because of the fantastic quality of care the teams provide there. So, when
I went up on the floor, this is the day after the WHO declared the pandemic,
and even leading up to it, I think around end of January, we were…
Someone had the foresight to dust off the pandemic plan, and we kind of had a
look at it in Jan. That was the sort of turning point number one is, we had not
updated our plan. We looked at our stock of masks. We had three days of N95 masks.
And we decided we better start doing N95 fit testing. So, that was like, a big
moment. Organizations do N95, particularly in long-term care homes, on
an annual basis, so this was not anything new, but fortunately, our Director
of Care had the foresight to do that. The second sort of shift was going up
on the floor and seeing the staff — and this was day one after the WHO
declared the pandemic. And we had masks, we were wearing masks, and you could
tell the fear in people’s eyes. You just look. I went up on the
floor and there was silence. Then there were tears, no one was talking, there were
tears. You could see the fear, you could feel the fear on the floor. The
staff were begging for universal masking. This is again, way
before any province in the country had instituted universal
masking. And I couldn’t tell them that we only have a two-week supply of
masks. Like, I couldn’t tell them that. Because if we instituted universal
masking, we’d run out and then we wouldn’t have any masks. So, having that
internal debate, and being able to look our staff in the eyes and say look, “We’re
going to have to just make do with what we’ve
got. And we’re gonna have to put our residents at the forefront, despite how
you feel.” The next day, I go back on the floor,
70 percent of the staff had left. Walked out, called in sick, went on
vacation. And, we’ve got two 25-unit sections with four staff total
managing. That’s not even enough staff to manage one 25-bed unit. And that’s when the
real panic started to kick in, and we went into overdrive.
Dr. McKinnon mentioned a quote from you that you
wouldn’t ask of your staff anything that you wouldn’t do yourself, and I know that
a part of the story you shared with me is that you went on the floor, and did
the work that was necessary, just because of that
shortage. I wonder about those sorts of decisions. I know that pressure
comes to both of you from above, as you’re trying to manage all of your
staff, so I wonder about a decision like that — how crucial it was and how you
think that that decision was seen by those that you were leading, John?
Yeah, so the overdrive was, we got to staff up. These residents aren’t
getting fed, they’re not getting changed. They’re not living their best lives. In
fact, they’re living their worst lives. And we know from the news what
happened to unfortunately, many long-term care homes, and that was top of mind. This
is before — I was like, this is a tragedy in the
making. And I’m not a clinician. I’m not even trained to be a personal
support worker. In fact, I realized the only skill I have is one of a
residential aide, which is to feed our residents, which I did in any way
possible to help. And then it was a call to action. It was a call across our
organization — we have an ambulatory surgical site, we have community supports,
we have a research arm. And I called a town hall and said, “Look, I’ve been on the
floor for 36 hours straight, feeding, doing labour, cleaning” — doing a lot of cleaning,
I think the floors were cleaner than my own floors in my own house at the
time. And I said “I’m on the floor, I — we need your
help. Who’s going to volunteer?” Twenty hands went up. We had a
research assistant, a clerk, someone from the finance team, three nurses from our
surgical division, which were amazing. Lined them all up, split up,
and got to work. I think that action alone spread to the families, who at the
time — I think people will remember no visits, no visitation to long-term care. You know,
the iPads, the faces against the window, remember that? The families heard about
this, and one family member proposed, “Why don’t we go in and work too?” And I said,
“That’s the craziest idea ever! You know, the union will
be against that, our lawyers will fight against that.” You know, a very
administrative response — can’t do that! I called the lawyer, called the union
steward. Within 24 hours, we had 20 family members on the floor working as staff, as
temporary part-time, earning $17 an hour as a residential aide. They already knew
the people on the floor, so they were more than happy to help out. You
know what’s amazing too, is all those family members donated those wages back
to the organization. They didn’t keep it. It wasn’t about the money, it was about
serving, and it was about taking care of their loved ones and the loved ones of
others. And that to me is what community is all
about. But it’s also, you know, an example of leadership, in knowing that
you had to get rid of these barriers. Like, that is on you.
To remove the barriers so that people can actually help. So, that is one of
those those visionary things that was happening during that time. Dr.
Morrison, we talked this summer about your team, and Dr. Aneesh’s
research talked about trust — about building trust. And I remember clearly,
you saying that there was a certain moment in which you felt that you had
pushed yourself too hard, and perhaps you had pushed your team too hard during
that. And that is in retrospect, in looking back. When you look back at
that, what do you think might have helped you in being aware that maybe the push
was just too hard? Is there anything that could have prevented that looking
back, that pushing way, way, way too hard for yourself and your
staff? Well, I mean I heard one of the staff say to me, you know, “I’m only
working this hard — like I’m staying here, missing my
family, here all weekends, late at night, because I see you doing the same
thing.” And that’s what I think — it means that I can be here too, because if I
didn’t see you working this hard, I wouldn’t be able to be here.
And at the time, I thought okay, well that, you know, this is how we trust
each other. We all work together, we support each other, but maybe, that was
a sign that I wasn’t doing what was best for
them, either. Again, in hindsight. But you
know, we talk about things that were not there before COVID. We did not
have the surge capacity that we needed to manage any kind of
crisis. And we certainly don’t have that now. And just at a time, I think –
and maybe this will come up later, I mean, but just at a time when we really should
be putting more resources and human resources to help make the system better,
it’s just when I have fewer staff than I ever did in the height of COVID. But we
really need to recognize that surge capacity. But that trust is really
important. And how we create trust with our teams, with the politicians
that we serve, with the public, and trying to make sure that we had regular,
open, transparent, honest communication
was really, I think, what I tried to do with the team, and with the
public. And that meant that we showed emotions
sometimes. And I wouldn’t recommend crying on TV because it’s sort of, not a
great look, but it happens. And it happened in front of senior
officials, it happened with my team, and it also happened in the public.
Because it is emotional, it is about fear. But I think in doing so, it
allowed for some really honest communication and trust. And at a
time when we all needed that. You know, I would highly
recommend if folks are listening, to go to the videos that
we shot with John Yip and Dr. Morrison (you knew I was going
to do that!), and have a look at their stories, because it’s
a very deep… stories of their own fears during that time, and I wish
that we had another hour to get into all of that, but the videos I think,
do a great job. Dr. Joseph’s research outlined three themes that
emerged in the research: a widening disconnect between healthcare
workers and leaders, a mismatch between words and
actions, and a misalignment of priorities was the third. And you know, I think
the pandemic set the table for these issues to emerge, but as you both
have said, these are issues that have been ongoing. It just so happened that,
you know, this is an opportunity to look at all of it, all at once. What methods
did you use to help maintain trust with those you were leading during such a
stressful time?
John? Yeah, I think the old phrase of “actions speak louder than words” really
played a key role. Same example as Dr. Morrison, if staff see you doing what
you’re asking staff to do, it models that type of behaviour. And it’s okay to be
able to be vulnerable, it’s okay to share your fears, which I did on a daily basis.
Because while I work in healthcare, I am not trained to do any of this.
Particularly when there were deaths, where funeral home providers weren’t
allowed into the homes, and two very tiny PSWs and I
would bag the body the individual. Not in a dark body bag that is typically done,
but in a transparent plastic
bag, and writing their name and time of death on their face,
while you see the face, and wheeling them out in the hallway — empty hallway, and
into the front, where there’s a little bit more staff, into the hearse
that’s waiting. The staff looked at me and
said, “I’ve never seen a CEO do this.” And I said, “well I’m not the CEO right now, I’m
here to help. I’m just trying to help.” Trying to keep everything together and
doing the manual, hard labour that our teams do every day. They see this every
day within — outside the pandemic. It has given me a huge appreciation for the
bedside care and the care that happens before people come in and when people
leave. And I think that perspective has made me a way better
leader in terms of really narrowing that gap that Dr. Joseph talks about.
Really saying things that I mean and will do. If I won’t do it, and if we aren’t
going to do it as an organization, I’m not going to say it. I’m not going to
commit anything. I’m not going to be that bobblehead leader, which I think I was
pre-pandemic. You know, and as a young
staffer, I would look at leaders and just roll my eyes at a lot of things leaders
would say. And I didn’t want my teams to look at me that way. So, I think really
getting into the trenches like Dr. Morrison did is one way of endearing
that trust. You know, you’ve done the hard work together. You’ve shared these
very intimate details about yourself, and you carry that through post-
pandemic. And I still maintain very close friendships with many of the staff,
some of them who are still at Kensington, others that have left, and ironically, some of
them have joined SE Health. I still maintain very, very close relationships
with them. We don’t talk about the pandemic. We talk about our families, talk
about life, the good things in life, even though we’ve experienced a lot of
not-so-good things during the pandemic.
Yeah. Dr. Morrison, what about you? You know, now you are still
leading the province, you still have your staff with you. What have you done to
help to maintain that trust and build that trust after such a
stressful time? Well, I mean during the pandemic,
it sort of became the phrase I’d finish every press conference with,
and it — people started wearing t-shirts and putting it on
billboards like, “Be patient, be kind.” And I’ve had to almost — I’ve put it up
so I can look at it every day to remind myself, because I really want to lead us
as a group, post-pandemic, with some of that
same thing. “Be patient, be kind” as we — and we had to be patient and kind
with ourselves because it was really hard. And I think even for me
personally, I underestimated how long it would take
me to sort of come out, and how much it impacted my own mental health.
And of course, the team that I work with, and have the privilege of
working with all the time. And so, I think as John
said, you have a different bond with people you spent that much time with, and
you worked with. And it was — even as a collective, as a population,
especially in, you know, through that first part — to have that
collective sense of what we were doing. We were all working together in PEI,
and as a team, to try to protect our community and our health care system.
And I’m not sure I’ll see that sort of collective action, and that thinking
about others, in quite the same way. It was — it was really amazing to see that.
And that cooperation between so many different partners, whether it
was restaurants, businesses, long-term care
facilities, and our team all working together and forging those partnerships.
And I — so those are the things. So, talking about how do we maintain that trust, it’s
about maintaining those relationships that were really important and that
helped us achieve some really amazing things
during COVID. So, how do we make sure that some of that can continue for the
months and years ahead as we struggle with a precarious health
system and increasing demands from our population? Yeah, for sure. I want to
open up the floor to questions but I do want to talk to — so the Q&A section is
right there, if anyone wants to drop in questions for John Yip and Dr. Heather
Morrison, we’re open to that right now. But I do need to talk about mental
health. Not for just — I know the two of you struggled yourselves
personally. I wonder if you are thinking about the mental health of your
staff and yourselves differently now that we’re in this long tail of the
pandemic. How are you thinking or rethinking mental health now? Dr.
Morrison, can I start with you? Well, I think healthcare workers,
including Public Health officials, were subject — besides all the hard
parts of the pandemic, and what the whole community was going through — we
were subject to some harassment, bullying, threats, and vitriol that
really we hadn’t always experienced before.
And I know that impacts us in a
terrible way. You had people at your door — like, protesting you at your door! I
mean, that is pressure! Yeah, we had loud protesters,
in groups with loudspeakers and drums, outside our windows here at the office
for days and weeks. We had people come to my home. We had RCMP, we had police
calling me saying, “There have been threats, where are your children?”
They told me I couldn’t go anywhere by myself. I didn’t go out to
eat with my family for almost three years, I didn’t go to a grocery store. I
mean, some of those are for me. But I think, you know, as
healthcare workers, there was so much kindness we saw, but we saw some
real hard things too. And we were subject to people or to some having
some threats and vitriol. Which I think, this is the time — so I think
about how can we protect healthcare workers and public health officials,
in terms of legislation, in terms of policy, before the next crisis. And, even
without a crisis, how can we do a better job? Because it is really hard,
what healthcare workers do, every single day. And we certainly don’t need that
added element to impact us. And it has long
repercussions, long-standing repercussions, when there is threats to
yourself or to your family. And we are doing our jobs, so we should be protected
and be able to do our jobs, in a very safe environment, and not be subject
to that. Yeah, thank you so much for sharing all of that. John, what about
you? Have you been thinking about mental health? You have a new
position now with SE Health. You’re in a leadership position once again. How
are you approaching mental health and how are you approaching your own
personal mental health after such a — after this
crisis? I would admit this… mental health and well-being for
staff, pre-COVID… maybe, was not the top three things that I focused on. I can
admit that publicly. You know, I think leaders have an idea that
it’s important, but you know you got budget pressures, you’ve got
government policy changes, you know, all the other things that take
up your time. And so, I will admit it was not in the top
three. In my new-ish role, it is number one. It is number one. It’s largely
with the sector that I work in now — home care and long-term care. Eighty percent of the
staff are racialized women. Many of our staff struggle to put food on the
table with the wages. They have families, they have cars to fix because it’s
home care, and they carry a burden. A burden of not just caring for
their clients, but the burden of taking care of their
family. And we, I would say broadly, as a healthcare system, don’t
really invest or pay attention to it the way that we should. And, it’s no surprise.
We see, you know, thousands of front line workers leaving the system. It’s why we have
packed ERs and hallway medicine. The crisis that’s faced in
healthcare is not just about underinvestment in new infrastructure,
new programs and services — there’s that. But there’s just been a massive exodus
of people that we ignored. In Ontario, there was a controversial piece of
legislation called Bill 124 which kept wages for public sector employees, and
was only just repealed by the highest court in the province last week. Well,
if your wages are capped and you’re working 36 hours, you know, serving the
public, and your wages are capped — and are purposely capped, why are you
working that hard? So you know, for me, and it’s very interesting. Yesterday was
a big day of three back-to-back meetings, six hours of
inclusion work. And we are, as an organization, going to invest in wellness.
And we have — when we look at our benefits now, it’s not trying to find the cheapest
plan. We’re going to invest in giving our staff the necessary supports they
need. Whether they need them or not, they should have access to
it. And so, we’re being very intentional about addressing
this. And then for me, personally, it’s interesting. Like, I kind of joked before
in the practice call that, you know, I blocked out — these three years I’ve
blocked out. And I was running the other day in the
forest, and I just stopped and started crying for no reason. Like, I couldn’t
understand it. I just really couldn’t understand it. It’s happened once before
when my father died. It was many years later that it happened, and I
realized I actually hadn’t talked about it. I didn’t want to acknowledge it, and
it just came out. And I went to talk to my family, and my partner’s in healthcare
too, and I told her this, and she just said, “I think you’ve got a bit of
post-traumatic stress symptoms.” Years later. And I didn’t even realize
it. And so, part of participating in this session, and with you in the
video series, and I’ve talked about it with you, Garvia, is that I didn’t really talk
about it. Didn’t feel the need to talk. I didn’t want to talk about it — I didn’t
want to do this! But I think I’m so glad that
I’ve participated. I’m glad there is being research being done on this.
It’s critically important to be able to share these thoughts,
experiences that kept bottled in. And I didn’t
realize what an impact it had on me until that run in the
forest. Yeah, thank you so much for sharing that. I want to just ask each
of you — we have a couple minutes left, each of you have about a minute for
this huge question that Dr. McKinnon has posed: What would you tell
future leaders who face these same challenges in the future? What would your
advice be? Dr.
Morrison? I was wondering if I had to go first. [laughs] You could just throw it to John,
if you really want. You’re allowed! I just — I just wanted to pick up –
before I answer the question, pick up on John. I mean, I think you’re so right.
Sometimes, I focused on thinking that other
people, wanting to make sure we had lots of sort of mental health debriefing,
for post-COVID, for teams and others, but I didn’t think I needed to participate in
them. So, I recognize that because I — and only later did I realize that
every time I talked about some of the issues, I would start to be super
emotional. Anyway, so I certainly appreciate that, John. I think one of
the things I would say to future leaders is
that our decisions always need to be balanced. So, the impact of our
public health decisions… I’m not sure we always
got the balance right, because it’s really hard. You’re trying to save lives,
but we also had huge impacts on mental health. And to be more cognizant from
the very, very beginning of those — that kind
of balance that we need to have going forward. I
think recognizing the need to have
the capacity built into our health care systems and public health
system, to manage these crises – which will continue to occur. And
because if we don’t have that surge capacity, with not enough people,
they work so much that it does impact their mental health, and then we can’t
continue. So, we will protect everyone better if we have
enough to manage in those surge situations. And then I think I mentioned,
the maybe — the final comment is around what we can that — it’s important to do
this research, to talk about it, to have these sessions. Even though I would like
to sort of not talk about it, sometimes, because I want to move on. But it’s
exactly what we need to do, so that we can learn, and that we can create
environments that make us more resilient, and
healthier, in this inter-pandemic period. And that includes
making sure that we are protected and don’t tolerate any kind of
bullying type of behaviour in any sense for us as healthcare
workers. Yes, thank you. John, you have a message to future leaders? It’s hard to
top that! No wonder why Dr. Morrison got a chicken named after her! [laughs] Thanks for going
first! She earned that! She did! Definitely, definitely! I would say two
things, and one is, use TikTok. And it sounds funny, but the point is this –
use the communication tool that the people you’re communicating to, will use
and absorb. We had done your typical PPE types of workshops, and people would
still not don and doff properly. And we came up with a 15-second TikTok video
of dance moves and so on, and guess what? Adoption rate of donning and doffing
went — like, shot up to a 100 percent. So I think as a leader, and I think Dr. Morrison does
it well, and her public health colleagues right across the country are amazing
communicators — they take very complex issues and articulate it in very simple
ways, so that the public can understand. So, number one is communicate well. Use
whatever mode is appropriate. In my case, since we had a younger workforce,
everyone was using TikTok. So communicate. Communicate often, simply, and
again, and again, and again. Number two, would
be — you know Jay-Z said this, when he accepted his Grammy,
and I completely, I subscribe to what he said. He said in accepting his award
is, “to show up.” And it’s as simple as that. As a leader, show up. Show up when
it’s hard. You don’t need to show up when it’s great. I think there, you allow
others to shine. But your job as a leader is to show up during those very
difficult, very, very uncomfortable situations, where bad news is horrible.
And when good news is great, let others take that on, and you can stand in the
shadows. But I think there are many people, still — leaders (that) don’t show up… don’t
show up for their staff, don’t show up for their clients or their patients.
And that’s not being a leader. So it sounds very simple. Jay-Z
has a way of being simplistic, but he’s a very, very intellectual guy. And
when you unpack that, there’s multiple dimensions about showing up. Showing up
as a friend, a family member, a leader, partner, father, whatever. Mentally,
physically, like it is very multi-dimensional. and I’ll let
everyone kind of gnaw at that, and what that
means. I love that. Maybe, Jay-Z was following some of the words of even
Winston Churchill from a long, long time ago. It just made me think of it. You
know, Churchill describes really anyone can — well, not anyone, but you can lead more easily
in good times. But it’s when things are harder, that it really takes true good
leadership. And I think that really is about showing
up. And it is when things are harder, that you have the leadership
that you really need. So, maybe Jay-Z and Winston Churchill were connected
some way. Let me tell you, two things I did not think were gonna show up in this
chat — Jay-Z and maybe Winston Churchill! I’m not sure, but I love that they both
came together, and I so appreciate both of you. John Yip, Dr. Morrison, thank you
for taking taking the time to be here, and be so generous in talking
about leadership in this way. I know it’s not easy to reflect back and
think about the things that you wish you would have done, but your generosity in
sharing your stories is just so appreciated in this forum. I even went
overtime! I’m only going to give people three minutes to rest and come
back, but thank you so much for this. And with that, I will leave everyone
to leave. Maybe we’ll give you an extra six minutes and
then we can come on back, and start our session again. So, see everyone
back here at about 1:05. Thank you, John, and thank you, Dr. Morrison. Thank you.
Thank you. Very nice to be back again with you.
Welcome back for those who are joining us or just joining today’s symposium.
It’s entitled “Navigating the fog: The role of healthcare leaders in
supporting provider mental health during the COVID-19 pandemic.” Now in our first
session, we were presented with findings from Dr. Aneesh Joseph. We
also spoke to two leaders in healthcare, John Yip and Dr. Heather Morrison,
who gave us firsthand accounts of what it was like to lead at the height of the
pandemic. It is so clear that in order to face the ongoing challenges — some would
call it a crisis in healthcare in the wake of COVID-19,
we not only need to hear stories but there also needs — we also need the
research. We need the empirical evidence. We need all of those things. To talk
about their research, we have some incredible leaders in research. Dr. Kim
Ritchie is here with us. Dr. Ritchie is an Assistant Professor in the School of
Nursing at Trent University. she completed a PhD in Rehabilitation
Science from Queens University, focused on understanding and identifying the
clinical presentations of PTSD and dementia in older veterans. Since
joining the Trauma and Recovery Unit at McMaster in
2020, she has also co-led the program of research that underpinned development of
our PHAC-funded Healthcare Salute initiative. To this day — I’ve
been working with you guys for so long and I still don’t know if I should say PHAC
or P-HAC. I need to get with the program. Dr. Jenny Liu is also here. Dr. Jenny Liu
is a post-doctoral associate with the McDonald’s Franklin OSI Research Centre
and an adjunct research professor in the department of Psychiatry at the Schulich
School of Medicine and Dentistry at Western University. Dr. Liu’s
background is in the science of stress and resilience — so important. She works
with stakeholders to identify the determinants of resilience in different
communities and supports efforts to promote or build resilience using a
number of evidence informed strategies and approaches. And Dr. Dayna Lee-Baggley is
also with us. Dr. Lee-Baggley is a registered clinical psychologist in
British Columbia, Alberta, Ontario, and Nova Scotia. She has an active research
program on behaviour change, obesity, chronic disease, professional
resilience, and acceptance and commitment. Again, if you have questions for our
research panel please put it in oh — P-HAC or PHAC, we don’t mind. Okay, thank you
Shannon! I will say it either way. If you have questions, please put it in the
Q&A portion. I’m sure you will have questions for these researchers. Welcome
to all three of you, thank you for being here. I think the best thing to do
right now, is just to ask each of you to give us just a little bit of a
Cole’s notes on — a little short synopsis of your research projects — and maybe just
a little bit about the findings and then we can go from there. Dr. Ritchie, can I
start with you, Kim? Is that okay? Yeah, absolutely. It’s so nice to be
here and thank you Garvia, for the warm welcome. It’s a real privilege to
be part of this panel and to be talking about such an important topic.
You know, Aneesh’s presentation and the the discussion that just happened with
John and Heather was so important and so moving. I just want to thank
them. So for our research, as part of the Trauma and Recovery Lab, we have been
doing research for just over three years now, talking to healthcare providers.
And we have now completed interviews with 126 healthcare providers from right
across Canada and we’ve collected surveys from over a thousand. And so
we’ve really, you know, come to learn a lot about what their experiences have
been through the pandemic. And I think one of the things that we’ve really
learned about that I think is relevant for the discussion today, is about
how impactful organizational support is on the mental health of healthcare
providers. And when I heard John specifically talk about how, you know,
prior to the pandemic I think we knew it was important, but maybe not in the
top three or in the top 10 sort of priorities. And so I think we’ve really
learned now about how important this topic really is and how much the work
itself really takes a toll on the mental health of healthcare providers. We all
spend a lot of time at work, but I think, you know, for healthcare providers they
they see a lot of really difficult, sometimes emotionally stressful things
as part of the work. And we don’t talk about it enough and I think that’s
been something that, now, we’re starting to talk about it a little more, which is
a really positive thing. Great. We are going to circle back and talk about your
findings shortly, but Dr. Liu, what about the — what
you’re up to with Revel. Sure! Thanks Garvia.
It’s a pleasure to be here today and you know, every time we talk about Revel I
kind of have to dial back a little bit and talk about kind of the background of
how we arrived here. So we’re also a P-HAC or PHAC-funded — thanks
Shannon! — we’re also PHAC-funded project and originally our research
centre specializes in military research. And so, what we set out to do was adapt
the resilience training for the military, the R2MR Program or the Road to Mental
Readiness Program, and adapt it for healthcare contexts using an
implementation science framework. So focusing on adoption, focusing on
implementation. And part of that process was identifying who’s, you know, our
target reach or target audience and then doing in-depth work with them to figure
out what are their needs, so that we can customize that adoption. And during this
process, it dawned on us very quickly, so Road to Mental Readiness is
essentially a program, you know, there’s modules, there’s kind of self-learning,
self-directed training, and all of those things. And our learnings were, you
know, in the midst of the pandemic and all of the sort of the subsequent
effects, healthcare workers don’t want any more modules. They’re already
inundated and overburdened as is and the last thing that anyone wants to do is to
take more time from their daily lives, probably not reimbursed, to log on to do more
modules and do self-directed learning. So that was kind of one of
the big learnings. And then also most of the stressors that were identified
during that process of deep discussions, were organizational in
nature. So it wasn’t a lack of awareness of mental health strategies, it wasn’t a
lack of yoga that was, you know, contributing to their organizational
burnout. It was very much the organizational policies, the rapid
changes, the feeling like your organization doesn’t have your back. All
of the things that we’ve just heard in the last hour — those were the themes
that emerged and that was why we couldn’t just say “Okay, let’s just stick
with our original plan, let’s adapt the R2MR.” So we want to actually shift our
approach and essentially want people to revel in the work that they do want them,
to re-engage with the organization. And how we do that is by working with
organizations to re-conceptualize and transform the way
that they think about well-being support. Right? Is it just that we throw a bunch
of, you know, individual-level things at these healthcare workers and some hit
and some don’t, and you know, and look at where they stick? Or is it that we
just transform the way we think about well-being and the role of the
organization and the role of leaders? And that’s very much the work that we’ve
been doing in the past two years. I love that. I love that because Dr.
Joseph’s presentation talked about a cultural shift and that’s what you’re
talking about. It’s not just the modules and teaching people, it is shifting
culture, which is — can feel like an iceberg, I’m sure. But we’ll talk about
that. Thank you. Dr. Dayna, can you tell us just a little bit about the work
that you’ve been doing? Yeah, thank you. Thanks for having me. So I’ll just
focus on the work kind of relevant for this topic. During — so I was a
front line worker during the pandemic. I was working on the medical, surgical,
and cancer care teams at the hospital. In Wave 1, I got redeployed to give therapy
for front line workers and medical first responders of the shooting in Nova
Scotia. And then in Wave 2, I was working in the cancer centre. And so we
got some funding to do burnout in front line workers with my colleagues at
St. Mary’s University, in industrial organizational psychology. And similar to
Dr. Liu, I was like, “We are not going to tell these people that they just need to
do more yoga or if they just did more mindfulness everything would be okay”
And so we chose to do leadership training, because leadership is a way
that you can address some system level problems and your fastest way of doing
that. And so we developed, you know, a training program. We’ve now tested it,
you know, in three randomly, you know, weightless designs, both in home
care workers as well as physicians. We did it during the pandemic, so in our
weekly data you can see “Here’s where Wave 3 hit of the pandemic” and
showed that we could reduce their own burnout, involuntary indicators of
stress like their resting heart rate, so that we could address some of those
system-level problems. The second thing that we did was we did an
intervention on moral injury for nurses. And so we are working with people
who work in the military, to work on moral injury. There was a lot about
that you know, potentially being a problem for healthcare workers and so we
did an intervention with them as well. And a lot of similar issues about –
that have been mentioned already, about the institution not being there to
protect them, the institution failing them. Those were often the sources
of the moral distress and the moral pain that people were experiencing. And
so, what we’ve really been working on now – as a psychologist, I spent most of my
time helping individuals, right? But then, somehow like, sending them back to toxic
workplaces, and I was like, “I really just want to fix some toxic workplaces for a
while,” and so we’ve really been working with workplaces on having comprehensive
mental health strategies. Which, for the record, is not an EAP, right? Those are
lovely, you should have them, for sure. But that is when the crisis has already
happened. So we focus on, “How do you put fluoride in the water? How do you embed
this in your everyday actions?” And so we think about, you know, trauma-informed
leaders, we think about psychological safety in the workplace — these are
the organizational factors that we need to address. You don’t want to rely on
help-seeking behaviour of employees, like — so we always want to empower employees,
but we really need to be targeting those systemic organizational factors and
that’s really what we’ve been focused on. And then lastly we just — I get so
frustrated, because they’re — when I started working in corporate land, they
just make stuff up — I’m not kidding you, like, there’s not a lot of research there.
So in healthcare, everything has to be evidence-based, like you have to, you know,
you don’t just get to make stuff up. But in workplace — like, mental health? There
are tons of people who have just come up with their own strategies, their own
ideas, it’s not tested, there’s no theory. And I was really shocked by that! And
so, it’s also become our mission of, like, how do we increase access to
science-based information? There’s a lot of good research and it is not getting
to the people who need it. There is like, this major delay between research and
implementation. And so we also work on that: How do we get more access to
people so that they can stop suffering? Like, we know a lot of ways to help
people and it’s really not getting translated fast enough into everyday
lives. That was like a mic-drop moment right
there, Dr. Dayna. Thank you very much for that. It is, you know, we keep circling
back to systems and I’m really interested in Revel and what
you are doing there, especially within the military, Dr. Liu. I had the
great fortune of talking to Major Beaucage, Marilou Beaucage, who led some
of the first teams that went to Wuhan and brought back Canadians. She’s just
this incredible leader in the military. But she talked about the
systems, she talked about the pressure that she gets from above and the need
for the whole kind of system to lock into place. So I’m
wondering about the — what is the most urgent need –
systemically, if you could just wave your wand Dr. Liu, and say, “This is what the
system needs.” I know this is a big question, but what needs to be addressed
urgently, right in this moment, before the next crisis comes? Oh, tough question.
So, I think I want to unpack that a little bit, right? So first, we’re
talking about, you know, the — all the work done in the military and
that’s a huge system, you know? Lots of different kind of channels, lots
of different moving parts, and an old institution, right? And take that
and apply it to healthcare and you’ve got the same challenges, right? You’ve got
bureaucratic channels, you’ve got like – you know, it’s institutions that’s been
around, and you’ve got a lot of moving parts with not a whole lot of cohesive,
sort of, glue to tie them together. And that’s really one of the fundamental
challenges, is that the system was inherently broken well before a pandemic
even hit, right? And any kind of lack of acknowledgement of that is not
true, right? We’re not — it’s not like pandemic created these problems, it just
magnified and amplified all of the challenges that we face now. So things
like shortages and resources, not having, you know, a wellness vision or wellness
strategy — all of those were in existence, and so that’s really the fundamental
challenge. It’s about how do we transform wellness and inject it
into this institution and all of its moving pieces? So Dr. Lee-Baggley, you
talked about, you know, a wellness strategy. That’s so key. That’s one of the
challenges we’re toying with anytime we’re partnering with an organization
and thinking about wellness at an organizational level. It’s — for some it
might mean that, you know, well-being or staff well-being wasn’t
even in a mission or vision statement. Now, if that’s the case — let’s just kind
of play that out, right? What does that look like? It looks like, you
know, at the highest, highest level, where a lot of these decisions regarding
resource allocations are being made, someone doesn’t have that within their
mandate to do so. And so then where do you squeeze out the time, the effort, the
resources, the focused attention, to attend to wellness, right? Someone,
somewhere down this cascade chain, needs to be responsible. And where do you see
that? And if that’s not a vision or mandate, how do we then highlight it and
and make others aware so that it becomes a strategic
priority? And in the presence of a priority, you know, what does that look
like? What does that strategy look like? I think you answer a
question right there that I’m going to pose to Dr. Ritchie about focusing
on leadership, because when you’re looking at the stream that’s coming down,
where can you — you know, where can you be the beaver to put in
the stop, let’s look at this first. And the beavers, in this case, are leadership.
It’s the leaders — this is why this is happening. So Kim, I’m wondering if
you can tell us what the research is telling us about the mental health of
the leaders themselves? Because there is — if we want to help these leaders to
implement these things, I think that there is a crisis — within the leaders
that I spoke to, for sure, in their own mental health. They’re having their own
mental health challenges. What were you — what were you hearing in your
research across the country? Yeah, I — that’s exactly it and
I think, you know, we interviewed front line, middle management, and senior
management, and I think they’re all struggling with mental health and I
think that, you know, the point about how things were already very broken
before the pandemic and things are just amplified now, along with this
amplification also of the mental health struggles across everybody. And one of
the things that we’ve been working on to try to address this within the
leadership is taking the idea of trauma-informed care. And I think, you
know, most healthcare providers are familiar with trauma-informed care,
because it’s something that we’re very trained to do for our patients and
clients. But it’s sort of taking that and turning that to the employees and staff
and people themselves and embedding that. And how do we embed that into an
organization and train leadership and train front line staff to embellish and
integrate these ideas of trauma-informed care? In the prior
presentation, we talked a lot about trust and I think that’s one of the really
primary things that we’re all talking about within the system, you know? How can
we develop greater trust and safety within our organizations and with our
leadership — between our leadership and front line and between each other within
teams? And I think that’s the real foundation of trying to rebuild these
connections and trying to rebuild the organization in a better way, hopefully,
than even before the pandemic. I think sometimes it, you know, it takes a crisis
to create these changes. And we’re really at this point now, where we’re — we
have to make these changes. So addressing this from sort of a systems
level of how do we look at the organization in embedding something like
trauma-informed care, but how does that trickle down to each level? And what are
the responsibilities then for the leadership within that? What are the
responsibilities at the front line? Because I think we all — in any organization, there’s
a responsibility for everybody to, you know, to integrate those types of
standards for each other. Well, that brings me to
that question of uptake, especially within leadership. Dr. Liu talked
about the fact that there is, you know, people don’t want modules.
They don’t want to spend the time, they don’t want to spend the resources, they
don’t want to — you know? But in order to implement some of this,
there has to be — it has to start somewhere and there has to be some kind
of uptake. Even Dr. Morrison, who we spoke to earlier, she said, you know, “My first
instinct is I want to move on, I don’t want to talk about this stuff anymore. We
need to move on.” And I think that that is a very natural, humanistic way of
thinking of a crisis, but that is not possible. So Dr. Dayna, I want to ask
you about the uptake in some of these programs that we’re seeing
coming out of this massive influx from PHAC to try and to create
these systems. What about uptake? Like, what is needed to jump that shark of,
“Here’s the stuff, how do we get people to just start using
it?” Yeah, the opportunity is that when people are in crisis, they’re more
willing to change, right? So a lot of the work we do is really on the behaviour —
like, the science of behaviour change — and so, for example, when we’re teaching
something about psych safety for leaders, we’re breaking that down into
behaviourally what does that look like? Like we have all these concepts of be a
trustful leader, be authentic, what does that look like? Behaviourally, what do
you need to do? And one of the things that we do in all of our work is why
is this important? We try to find value-driven reasons for change. And in
our theoretical models, values are about what you want to give to the world, not
what you want to get from the world. So they’re about how you want to show up,
right? The kind of leader you want to be, the kind of employee you want to be, the
kind of partner or parent you want to be. And so we’re always trying to find that
motivational reason for change so that it doesn’t become a check the box
kind of activity. When you can find value-driven reasons for change, then
you know, it’s a sustained change. So there is a ton of data on the ROI when
you invest in mental health. Like, there’s just a huge amount of data saying if you
invest in mental health, your numbers look better, your productivity is better,
your retention is better, right? But sometimes that data isn’t enough. I think
we also need to talk to leaders about what kind of legacy do you want to leave?
How do you want to be seen as a leader? How do you want to be known or
recognized? Because when you start caring about people’s wellness and their mental
health, then people start being loyal, people start wanting to do, you know,
extra. They want to be there and they’re well enough to stay, right? I left after
Wave 2 for my own burnout reasons, right? And you know, that maybe was, like,
a canary and the coal mine, but also we never said the canaries had to be more
resilient, right? Canaries in the coal mine is that, like, the environment is
toxic, right? You need to fix the environment. And so, I think we need to
start thinking about — again, there’s a ton of science of behaviour change. How do you
get people motivated? How do you get people ready for change? How do you
support them in the behaviour change aspects? Both for employees and
for leaders — and for organizations — about who they want to be. There’s a huge HR,
you know, crisis in healthcare, where there’s not enough people to do
the work and we’re just burning out the people who remain even faster. And so we
need a radical shift in terms of what kind of organization do you want to be,
how do you want to be seen by your employees, and making wellness — you
know, as the previous speakers said, like, the top priority. Like, employees are
always going to be your most valuable resource and we actually — you know, prior
to the pandemic, we would apply for research on resiliency in healthcare
workers and we wouldn’t get funded and the feedback was this isn’t patient
focused enough. So taking care of your employees, your staff, your healthcare
workers, isn’t patient focused enough, right? We need to see these not as separate
things, but what you need to do, to do good patient care, right? So we talk about
when you’re well, when you’re charged, when you have energy, who benefits from
that? It’s not just you, it’s also your patients, your colleagues, probably anyone
you interact with. Because, you know, we’re less grumpy and so we need to connect
these motivational reasons for change. And again, there’s a lot of science we
could be using to help make those changes.
Yes! I would just love for either one of you, Dr. Liu or Dr. Ritchie, to
jump in on this, because I think there’s a lot to build on here, in
talking about how we jump it into actual action —
implementation of these things. Dr. Ritchie, can we just start with you? I’ll
throw it at you. The implementation of the systems that
need to be in place. How do you see that rolling out, having done the research and
now seeing what leaders are thinking and feeling? Are they ready for it? How does
it happen? Yeah, I think that’s such a great
question and it’s so — it’s such a hard answer at the same time. I think — you
know, I think we’re in a space now where there’s this — I think you said it too,
where this — a sense of “Let’s just get on with it,” and, you know, “The pandemic’s
behind us, we’re just going to get on with it. We’ll do things the way that we
have done them before and we’ll just get going along that same train.” And I think
it’s really hard to stop and to say, you know, we’re not going to do it that way,
that we’re going to intentionally make a new change. And I think that that takes a
lot of courage, that takes a lot of — that’s kind of a really, sort
of, hard place for people to be in. So I think we have to sort of start
showing that there is something to be gained by doing these types of things,
that there are positive outcomes that we can build on, and that employee mental
health is a not just an individual responsibility but an organizational
responsibility. I think, you know, we’ve all talked about the research — we’ve all
talked about our own research and the wider research that really shows
that mental health of employees — if you have better mental health, you don’t
have the turnover. You have higher retention, you have better patient
outcomes, you know, we have seen that in our own research. Where we have many
healthcare providers — about one in two — saying that they are intending
or have an intention to leave their organization and/or profession. And so
these numbers are staggering and they’re really scary! You know, one of the
turning points, I think for me, during the pandemic when I was learning about what
was unfolding, was in conversations that I had during interviews and
healthcare providers said, you know, “The pandemic’s taking a real toll on my
mental health and my family, my friends, are all saying, you know, it’s time for me
to leave. I need to walk away from my job, but I don’t want to leave. I want to be
here and I’m really good at my job, but I need my organization to help me to do my
job better and to keep me here and to take care of my mental health.” And so I
think, you know, if there’s any sort of first thing, it’s that idea of leadership
in an organization prioritizing the mental health of their
employees. And I think Dr. Dayna mentioned that as well, is that has to
become the first step that we have to do. And I think by showing, you know, through
resources, through changes in the way that we connect and deal with
each other, by offering more than just EAP — offering more resources. There’s a
lot of healthcare providers who have no mental health resources or extremely
limited. And I think those are the places where we can really start to
build trust, to build connections, and to show this type of caring that we need to
do to build our biggest resource in healthcare,
through our employees. And in turn, as others have said, then we’re going to
really help our patients too. And we’re going to be better humans in our
personal lives and our professional lives, for sure. But are leaders buying in? Like,
are you getting to the people that need to be reached in order for this
change to happen? I think that that’s where I’m getting stuck, personally, in
listening to everyone. Is it getting to the right people? I think Dr.
Morrison and John Yip are — they might be exceptions, I’m not sure. But I’d
like to know if the work that you’re doing is
getting to the right people. Dr. Liu? Absolutely. That’s an
important question, and you know, working with our partner sites in the
project that we do, and whether we’re speaking with middle management or
whether we’re speaking with, you know, C-suites, executives, the CEOs… the
messaging is the same from them. It’s that they care, they want change to
happen, they recognize that there’s challenges. Where the disconnect often
comes from is from, you know, the — kind of the different levels, right? As it
trickles down, things are not necessarily communicated. So even from the earlier
session this morning, we hear about difficult decisions being made and rapid
changes, and those kinds of decision making and the kind of struggles are not
communicated in a transparent way. And so that’s where the cultural shift is,
that’s where the front line feels like no one has their back. While their
leaders, might be trying very hard working with the limited knowledge, the
limited resources that they have. And so solutions of yesterday, right, where we
focused on, you know, individual levels, where we focus on, you know, doing
patchwork here and there and trying to fix the solutions, they’re not
going to actually help share that information and bridge the gaps. And so one
of the the things I’m hearing from both Dayna and from Dr.
Ritchie is that the struggles of yesterday, like getting funding for
a project that focuses on implementation, that focuses on the employee experience —
you know, those things are not — they weren’t funded before, but
now they’re being recognized. And so one thing I want to highlight is that, you
know, what got us here to this point is not going to get us to the next stage.
And so, transformative change is required. Change is required, meaning that,
you know, whether it’s funding opportunities, they need to recognize
it’s not about a simple pre-/post- intervention design anymore. It’s about
implementation, system transformations. And we’re starting to see from
researchers’ perspectives more opportunities that are geared towards
that type of setup, right? At the beginning, even when we were doing
a lot of our projects, the funding opportunities didn’t look like what it
did now. And it’s going to take elect change on the leadership side. They’re
also now recognizing that it’s not just a top-down decision model that’s going
to, you know, have the maximum impact on employee well-being. It’s going to take,
you know, a horizontal approach where people feel represented. Where front line,
the staff, the people that are on contracts – everyone, as part of an
ecosystem — feels like they’re seen, feels like they’re heard, feels like they’re
valued. And that’s the type of solutions that need to be designed and pushed
forward for things to to change.
Thank you for that. And again, just to reiterate back to your question, leaders
want those type of solutions. Leaders are open to hearing about the evidence. And,
you know, there’s tons of that available. It’s just about how do we translate that.
And here, we kind of go back to communication, right? It’s about that
communication. How do we communicate decisions? How do we communicate that
leaders care and that things are being done? Are being planned to help?
And that we want to transform — we want to change. You know, that beautifully brings
me to a question about the next steps in your research. Where the
research needs to go next, and how the next steps in
your research will build on what you’ve already — on the momentum that you
have with each of the individual projects that you’re working
on. So what happens next? What
would you ideally — it sounds like there is a buy in,
this is a great time. You know, as we’re — as Dr. Morrison, said we are inter-pandemic —
we’re in the inter-pandemic period, right now — thank you for that. And we’re
preparing for better responses for whatever comes
next. What is the next phase in the research that needs to be
implemented? And I’ll start with you, Dr.
Dayna. Yeah, for sure. So you know, we actually partnered with a tech company —
we created a tech company to create a scalable, science-based solution. And so
we came up with an app — because that’s a nice, scalable, science-based solution
that’s full of science called Impact Me — and the resources is in the chat.
But we did that because we feel like we have enough — the science
in our app is based on a thousand randomly controlled trials of how this
therapy, you know, impacts a wide range of things. And it’s, you know, out of my
comfort zone to be like a co-founder in a tech company. It’s not something I ever
envisioned, but I would — like, my mission in life is to help reduce human
suffering and it’s not going to happen through one-on-one therapy, right? That’s
why — that’s partly why I left the hospital. I was doing one-on-one therapy
with cancer patients, clearly a deeply meaningful thing to do, but the mental
health needs of the planet had gone up in Wave 2 and I was like, one-on-one
therapy is not going to cut it. And so, there’s a lot of science. We need to be
implementing it, we need to be partnering with people who know how to get these
systems into corporations, into organizations, into hospitals, into other
places, so that we can actually start having an impact with all this knowledge
that we already have. And so that’s what we’ve come up with as a solution to,
again, increase access to science-based information. And I think that it is
this, like, implementation — partnering with people who know how to do it. Researchers
actually are not great at it, because we’re great at the research, but that’s —
it’s not our skill set to necessarily, like, you know, bring it to the people who
need it. And so we need to be partnering with the people who do know how to do
that to, like, get it into the hands of the people who need it
most… Of course, I have to do that every Zoom, at least. Every Zoom I have to do at
least once. Are you seeing some of that happening? Is it getting into some hands?
Is it in action and what does that action look like?
Yeah. So, you know, we have, you know, an early version of the app available.
And so we start the conversations. And really, this is from a motivational
perspective, you know, from clinical psychology. You start with the people who
are most ready. We talk about it like a traffic light: you can be green light
you’re ready, yellow light ambivalent, red light not ready. Start with the green
light companies! There are companies — and I would not actually describe
healthcare as being one of the ready companies. They’re a little more
yellow light and red light. But there are other organizations who have
absolutely bought into mental health being important for their employees and are
willing to invest into their employees. And so we start with them — we start with
the people are most ready. They — you know, healthcare is always in a crisis
and so they can never be forward thinking. They can’t — they often are not
proactive, because they’re always dealing with the crisis. And I hope that that
crisis helps motivate them to do something different. Healthcare,
you know, and like in lots of places — certainly in my province — kind of looks
like a dumpster fire. But I’m hoping that maybe if it just burns down, we can build
something better. Because the culture needs to change, the attitudes need to
change. And I’m hopeful about that because I think we can be hopeful in
possibilities, right? That there is such a crisis now that maybe people will
start investing in their employees and trying to retain them, and not just, you
know, think that you can just find as many workers as you need. And so we get
lots of good feedback, you know, because the app is dealing with burnout —
burnout for leaders and burnout for employees. So again, we’re targeting
those system-level problems through leadership training. We get lots of good
feedback on it and, you know, we’ve created it in a way that is viable to be
scalable to help a lot of people. And so, yeah, ask me a year from now how
it’s going? Hopefully it’ll be really great and everyone has access to it.
Again, to us — to me, it’s about helping to reduce human suffering and increasing
access to science-based information. And so, taking a big leap out of my comfort
zone as a researcher, to then try to offer something that’s viable to the
public. That’s great. I want to open up the floor to questions, as well, for
our researchers. So the Q&A tab is there for you. If you have
questions, please put them in the tab. Dr. Ritchie, I’m going to continue the
conversation with where you see the research going for the Trauma and
Recovery Lab. What needs to happen next? This is a big chunk that you’ve bitten
off, a lot of interviews being done. What happens
next? Yeah, so that’s such a good question. And so, I think, you know, we sort of
are taking sort of a multi-prong approach. I think for our next step, we
have learned a lot during the pandemic. We’ve talked to a lot of
leaders, a lot of front line healthcare providers, and I think now it is
about implementation and evaluation. So, you know, taking what we’ve learned,
especially around things like the culture change and the culture shift
that I think we’ve all talked about today, the trauma-informed care lens that
we have learned a lot about — what are the barriers and facilitators to
implementing those types of principles into an organization? And how do we go
about implementing that and scaling it up? And then I think really
importantly, evaluating to see how are these things actually working for the
organization and are they making the types of changes that we’re hoping to
make across the board? So I think that for us, in the Trauma and Recovery Lab,
that’s one thing that we’re really focused on and thinking a lot about is
how do we implement some of these things. We’ve also — the other thing
we’re working on is trying to put together a lot of resources for the
front line healthcare provider who’s struggling and just wants things —
and for the leaders! And so we’re trying to tailor different resources for them,
through our videos and through other things so that we are coming at it from
a couple different ways. Looking at it from a structural — a structural
way, but also for the people that are, you know, working day to day and just need
some of those resources and help and want to see themselves. You know, the
the most — the worst thing is to feel like you’re the only one who’s struggling. So,
I think by, you know, starting these conversations, like this symposium today,
and through all the work that everybody’s doing, I think it’s starting
to make that feeling of “They’re not so alone.” Thank you for that. Dr. Liu, what
about the next steps for the Revel project and for research in
general? You know, we are not out of it. There is going to be other waves,
other crises. What needs to happen next?
Where do you want your research to go moving forward? Absolutely. And it’s — no, my
answer is not going to be dissimilar to what Dr. Ritchie, Dr. Lee-Baggley said.
You know, change is uncomfortable. Change is uncomfortable, especially when
we’re working with system transformations. And one of the things
that we’re really trying to work hard at is, how do we make make these efforts
evergreen? How do we sustain and maintain this momentum of change, right? When
crisis hits, everyone’s motivated. Everyone recognizes that, you know, things
need to happen, things need to change. But when things get better, that’s when we
often default to what was comfortable — what was known. And so the the challenge
has always been, right, when we’re working with an organization, how do we embed
ourselves to help them, but have them remain autonomous in the way that they
maintain and sustain these transformations? So working with them to,
you know, asset map their available programming, to transform their vision
for well-being, to help them understand what are the roles- what are the
transformations, setting up short-term/long-term plans — those are the things
that we want to support organizations in doing, but not directly do for them. And
then at the same time, take — taking the learning along the way and
embedding it back into what we call a Revel framework, which is really a set of
methodologies for working with organizations. And so that’s what we’re
continuing the work for, and we hope that, you know, this kind of work
will continue to be prioritized. Whether it’s by funding, whether it’s through
communications, through, you know, channels like this where we have a panel talk to
get this information out to others. We hope this is a topic that continues to
be prioritized. Mhm. You know, there’s a
question here that I think is really important. We have a couple of
minutes left and I want to think about this question, because there
are — right now, we’re probably, you know, everyone in this room — “this room” — we’re
preaching to the choir. Everyone is kind of on the same page. We’re here because
we want to talk about a very specific thing. But if you’re a front line worker
and you’re hearing about the research that you’re doing and the app and all
these things that that can be implemented by their
organization, how does a front line worker encourage or push forward the idea
that change is needed? They have to talk to their leadership about it — it’s
just a whole other level of pressure for a front line worker to have to say, “These
things are out there in the world, can we think about them?” So what kind of advice
might you give someone like that, who wants to see Revel somewhere, wants to
see the app, you know, wants to get that research into their
organization? What kind of advice would you give them? Who wants to
start? This is the only time I’m going to make you guys decide — the only time — for
the last question. Yeah, I can take a crack at it, since you mentioned Revel
first. You know, one of the things — going back again, change is
uncomfortable, but you know, solutions need to make everyone feel seen, feel
valued, feel heard. And so, as a front line worker, sometimes the first signs of
burnout comes from, you know, feeling not as attached, feeling
disengaged from your work. And actually, the opposite of burnout is not
necessarily resilience, right? It’s about meaningfully engaging with the work. And
so, sometimes it just takes conversations — whether it’s with your
manager, whether it’s with your colleague about things that are happening at work.
And so we can, you know, initiate some of the sparks that will lead to some
transformations or some discussions, right? Baby steps here. But it’s about
not disengaging, about taking a step
in leading with, you know, what you value, right?
And starting that conversation. That’s great, thank
you. Dr. Dayna, go ahead please. I’ll add that which is, you know,
one, connect with other people. You know, an individual can only make system level
change with other individuals, so connect with other people who believe the same
things as you do, that are thinking the same way, so you have that support.
Because groups do make change and they make change all the time, so don’t be
hopeless about it. It happens all the time. Think of all the things that we
have changed in the world, right, through groups deciding that they want
to change. The other thing you can do is to model the behaviour yourself, right? We
had some great role modelling by leaders today, about being vulnerable, about
sharing their challenges, about being authentic. So, you know, we can role model
wellness ourselves, which sometimes, in healthcare, is about placing boundaries.
It’s about, you know, recognizing that my well-being is in the service of my
patients well-being. That I can’t, you know, I can’t be unwell and really serve
patients well. And then finally, this is what leadership is. Leadership is
making the hard choices. You know, character is who you are when it’s hard,
not when it’s easy. And so leaders need to step up and say these changes need to
happen. And you need bottom up and top down to make these kinds of changes.
Leaders need to step up and say, “We’re just going to do it. We’re going to do it
and we’re going to support people through this change.” And it’s necessary
because that’s exactly what we need to have happen and that’s what real
leadership would be. Yes. Dr. Ritchie, you have one
minute. Yeah, I think, you know, very similar — same lines. I think, you know,
working together with your peers, trying out what works for you within your peer
group, and then scaling that to others in your unit or in other units, or taking
that to your organization. I think those types of stories, of saying, you know, “This
has worked well for me, you know, why don’t you try it?” And then it just starts
to build and it becomes a momentum of its own. And then if you have a group of
people who are able to say, you know, “I’ve tried this app,” or, “I’ve tried this
particular type of website and this is where I go to get my resources.” Those
stories are very powerful and I think that’s a way to engage others in the
conversation and ultimately engage your leadership and your
organization. I think everybody’s looking for answers and I think these are types
of ways that we can, you know, give our own testimonies of, “These are the things
that are working for us,” and that’s very powerful, I think, for an
organization to hear. Amazing. Thank all three of you so
much for your generosity, your knowledge translation, which I think
is such a key component for organizations — having all of this
research and then being able to translate it into a way that makes
sense for folks to implement is is huge. So I want to thank you all for
taking part right now. And for those in the audience at this symposium, who
took part — a very lively chat happening. I love this one from Daniel that says
“Dr. Liu said it correctly, staff do not need more modules. Enough is enough.” Yes!
You know, thank you for everyone taking part and being really open to
these conversations. I appreciate it. I’d like to now welcome Dr. Margaret
McKinnon back for some closing words on this symposium. Thank you all,
again. Thanks so much everyone. I want to just offer our most heartfelt
thanks to everyone who participated today. To hear the stories
of leaders and to hear the personal costs that came with their sacrifices,
and also what we can learn from what happened in the past to make a better
emergency and pandemic response for the future. Thank you Dr. Morrison, thank you
John for sharing your stories. We could not be
more grateful to you. I want to also thank our expert panelists and just to
say that, again, I think as Dr. Morrison talked about, we’re in that inter-
pandemic period or inter-crisis period right now. And I think there were a lot
of lessons that were learned as we started to mount a response to the onset
of the pandemic, where we didn’t have enough PPE, we weren’t prepared with
psychosocial or psychological responses for healthcare workers, public safety
personnel, our military members, our Veterans, and even for the public. And
you know, as we have this maybe grace period that we’re in right now, how
do we move forward to ensure that the next time we’re ready? Because we had the
SARS pandemic, and I think we learned a lot, but we didn’t always take the
opportunity to leverage those lessons. If we can do so now, we’re going to be so
much farther ahead than next time this happens. But all that said, you know, I
think we can reflect on the systems level, but we also need to reflect on the
individual level. So, thinking about the individual sacrifices of healthcare
leaders, the sacrifices of their families, the sacrifices of the front line. I
think when we think about how do we recognize that, we recognize the
individual and their contributions, and then we recognize at the systems level,
as well, what we need to do change that system. I think it’s just a remarkable
conversation and I just want to thank everyone so much. And I want to end by
also thanking Cristina Stef, Sangita Singh, Andrea Brown, and many others in
the Trauma and Recovery Lab who contributed to putting this
information together into the whole of the project. Along with Garvia,
Make Things Well, and others. I just want to say thank you from the bottom of my
heart. At the end of this, I just do want to say, we salute you, Canada’s
healthcare workers and leaders. And we thank you for your
service and for your sacrifice, just as we would to military members and
Veterans who have stood in similar war footing over many, many generations in
Canada. This was another generation that faced that challenge and we’re so
grateful to you, so thank
you. Thank you, Dr. McKinnon, and thank everyone else. Thank you everyone for
taking the time to be here today. We hope that you are leaving with helpful
takeaways. Thank you for taking part in the chat. If you want to leave one word
in the chat right now about how you are feeling about this session, please do.
Half of you have already gone, but if you want to just drop something in here, just
to — a word of appreciation for our panelists today, taking the time and
putting in the effort to chat with us. Thank you again for joining, have a great
day, and Dr. McKinnon — last word is yours. One last thing: We must thank the
Public Health Agency of Canada, as well, for their support of Healthcare Salute,
of the symposium series, and for really the efforts that were mounted, as well, to
support all Canadians. So thank you to the Public Health Agency of Canada, as well.
And to our healthcare workers, our front line leaders, and our front line staff, thank you.
Host

Dr. Margaret McKinnon, Homewood Chair in Mental Health and Trauma; Professor, McMaster University
Dr. Margaret McKinnon is Full Professor and Associate Chair, Research in the Department of Psychiatry and Behavioural Neurosciences at McMaster University, where she holds the Homewood Chair in Mental Health and Trauma. She is also the Research Lead for Mental Health and Addictions at St. Joseph’s Healthcare Hamilton and a Senior Scientist at Homewood Research Institute.
Work in Margaret’s unit focuses on identifying the neural and behavioural correlates of PTSD and trauma-related illnesses and on translating this knowledge to the development and testing of novel treatment interventions aimed at reducing the cognitive and affective sequelae of these conditions.
A licensed clinical psychologist and clinical neuropsychologist, Margaret has a special interest in military, veteran, and public safety populations (including healthcare providers), and has worked with these groups clinically and in her research program. She has published or in press nearly 150 scientific works.
Under Margaret’s leadership, the Trauma & Recovery Research Unit is supported by federal and provincial funding from the Public Health Agency of Canada, Canadian Institutes of Health Research, the Canadian Institute for Military and Veterans Health Research, Veterans Affairs Canada, Defence Canada, the PTSD Centre of Excellence, MITACS, and the Workers Safety Insurance Board of Ontario; by a generous donation to Homewood Research Institute from Homewood Health Inc.; and by generous gifts from private foundations including True Patriot Love, the Cowan Foundation, the Military Casualty Support Foundation, the FDC Foundation, and the AllOne Foundation.
Margaret is a frequent commentator in the media on matters related to PTSD, moral injury, and the impact of trauma on special populations.
Healthcare leaders

Dr. Heather Morrison, Chief Public Health Officer, Prince Edward Island
Dr. Heather Morrison was appointed Chief Public Health Officer of PEI, Canada in 2007. As Prince Edward Island’s first female Rhodes Scholar, she completed Master’s and Doctoral degrees at the University of Oxford. She returned to Canada for her medical degree from Dalhousie University, followed by specialist training in Public Health at the University of Toronto. Heather has completed a Master’s certificate in Physician Leadership from Schulich Business School at York as well as completing a certificate program in Media & Medicine from Harvard Medical School.
As Chief Public Health Officer, Heather has provided steady, trusted, and visionary public health leadership during public health emergencies such as the COVID-19 global pandemic as well as issues such as opioid use and chronic disease risk factors. Heather chaired the Canadian Council of Chief Medical Officers of Health for 5 years and has served as PEI’s representative on the Public Health Network Council of Canada and its Special Advisory Committees.
Described by one well-known local broadcaster as “grace under pressure”, Heather is known for her open, transparent, and clear approach to decision-making, relying on the best available evidence to try to protect and promote the health of Islanders and Canadians. She considers collaboration, professionalism, respect, and empathy to be the hallmarks of her approach to leadership.
Heather has been recognized with the distinguished alumni award from the University of PEI, Dalhousie University Medical Alumni award, the distinguished alumni of Canada Games Hall of Honour and an honorary Doctor of Laws from UPEI. In recognition of her exemplary public service, she was awarded both the US Consul General’s Award for Public Service by the US State Department and the Order of PEI.
Heather lives in Charlottetown, PEI with her husband and four children.

John Yip, President and CEO, SE Health
John Yip is the President and CEO of SE Health, a not-for-profit social enterprise bringing excellence and innovation, and hope and happiness to home care, seniors’ lifestyle, and family caregiving – to forever impact how people live and age at home.
John brings a broad, dynamic, and impressive range of experiences to SE health every day that includes community, business, equity, diversity, and inclusion, and over two decades of leadership experience in the health sector – all underpinned by a ‘serving with the heart’ approach. He is well positioned to build on SE Health’s exponential growth and expansion in the last several years and continue to grow the organization’s social impact in the areas of Indigenous health, end of life care, and caregiver wellness and support.
John’s commitment to community advancement is evident throughout his career, and especially in his recent stint as President and CEO of Kensington Health, a diversified not-for-profit community-based health services provider. John’s ability to deliver impactful care to communities while remaining mission-focused with an entrepreneurial spirit fuels his motivation to take SE Health into the future with extraordinary passion and purpose.
As a transformative, values-based leader, John continues to advance SE Health’s vision to forever impact how people live and age at home through its business of caring, social impact, and strategic investments. This includes providing innovative leadership in the home care space and helping to shape a new vision for aging across Canada and around the world.
Visit sehc.com/about/meet-our-ceo to learn more about John.
Research presenter

Dr. Aneesh Joseph, Postdoctoral Fellow, Trauma & Recovery Research Unit, McMaster University
Dr. Aneesh Joseph is a postdoctoral fellow at the Trauma and Recovery Research Unit at McMaster University. He holds master’s degrees in psychology and sociology. He completed his PhD in Sociology and Social Policy from the University of Southampton, UK. He has done ethnographic research with marginalized groups such as Indigenous communities as well as with institutions of higher learning. Understanding and augmenting change in individuals and communities has been the central concern of his research and practice.
Aneesh has clinical experience of working with individuals who struggle with mental health and addiction. His wide-ranging experience in group work and program development has evolved into a passion for group treatment in trauma and addiction. He has extensive experience of using meditation and mindfulness practices in helping individuals to lead grounded, purpose-oriented, and meaningful lives.
In the years he worked in higher education in India as a lecturer and an administrator, Aneesh gained invaluable experiences in supporting students and in managing funds and staff.
Panelists

Dr. Kim Ritchie, Assistant Professor, Trent/Fleming School of Nursing
Kim Ritchie is an Assistant Professor in the Trent/Fleming School of Nursing and an Assistant Clinical Professor (Adjunct) in the Department of Psychiatry and Behavioural Neuroscience at McMaster University. She completed a Ph.D. in Rehabilitation Science at Queen’s University, and a post-doctoral fellowship at the Trauma & Recovery Research Unit at McMaster University.
Dr. Ritchie’s research focuses on trauma and moral injury in healthcare providers, public safety personnel, Veterans, and older adults. For the past three years, she has been co-leading a national study exploring the mental health impacts of COVID-19 on healthcare providers and public safety personnel in Canada. Key contributions from this project have been the development of an evidence-informed treatment program and psychoeducational resources for healthcare providers and public safety personnel.

Dr. Jenny Liu, Head of Scientific Development and Knowledge Mobilization, MacDonald Franklin OSI Research Centre
Dr. Jenny Liu is a Postdoctoral Associate with the MacDonald Franklin OSI Research Centre and an Adjunct Research Professor in the Department of Psychiatry, Schulich School of Medicine and Dentistry at Western University.
Jenny’s background is in the science of stress and resilience. She works with stakeholders to identify the determinants of resilience in different communities, and support efforts to promote or build resilience using a number of evidence-informed strategies and approaches.

Dr. Dayna Lee-Baggley, Registered Clinical Psychologist; Director, Dr. Lee-Baggley and Associates
Dr. Dayna Lee-Baggley is a Registered Clinical Psychologist in British Columbia, Alberta, Ontario, and Nova Scotia. She is the director of Dr. Lee-Baggley and Associates, a virtual health psychology clinic specializing in clinical interventions, training for healthcare providers, and research in health-related issues (e.g., chronic pain, sleep, COVID burnout, PTSD for point-of-care workers).
Dayna worked for almost 15 years in multidisciplinary teams on medical, surgical, and cancer care hospital units providing assessment, therapy, and consultation for patients with chronic and life-threatening health conditions. She also conducts research as an Assistant Professor in the Department of Family Medicine, with a cross appointment in the Department of Psychology & Neuroscience at Dalhousie University and an Adjunct Professor appointment in the Department of Industrial and Organizational Psychology at Saint Mary’s University. She has an active research program on behaviour change, obesity, chronic disease, professional resiliency, and Acceptance and Commitment Therapy.
Dayna has over 45 peer-reviewed publications and over 130 scholarly presentations. She is a Senior Consultant providing healthy workplace interventions for employees, teams, and leaders with Howatt HR Consulting and the Chief of Research for the Howatt HR Applied Workplace Research Institute. She is an internationally recognized trainer in Acceptance and Commitment Therapy. She was the recipient of the 2017 Women of Excellence Award for her contributions to health, sport and wellness (Canadian Progress Club Halifax). She is the author of the book Healthy Habits Suck: How to get off the couch & live a healthy life…even if you don’t want to.
Moderator

Garvia Bailey, Co-founder, Media Girlfriends
Garvia Bailey is a co-founder of Media Girlfriends Inc. Her career in media spans close to two decades as a producer, host, and columnist for the CBC and JazzFM. She is a co-founder of jazzcast.ca, a 24-hour streaming service that amplifies the roots of jazz as an African-American–derived artform.
Garvia is the recipient of the 2019 RTDNA award for opinion writing and a 2017 Silver Medalist at the New York Radio Awards. She is a jurist for the prestigious Canadian Hillman Prize for investigative journalism. Her work is centred around inclusion, care, and excellence in journalism.
With gratitude to Ward 1 Studios and Virtual Producers for producing this event and broadcasting its video feed.
Symposium 3: Navigating the fog Read More »