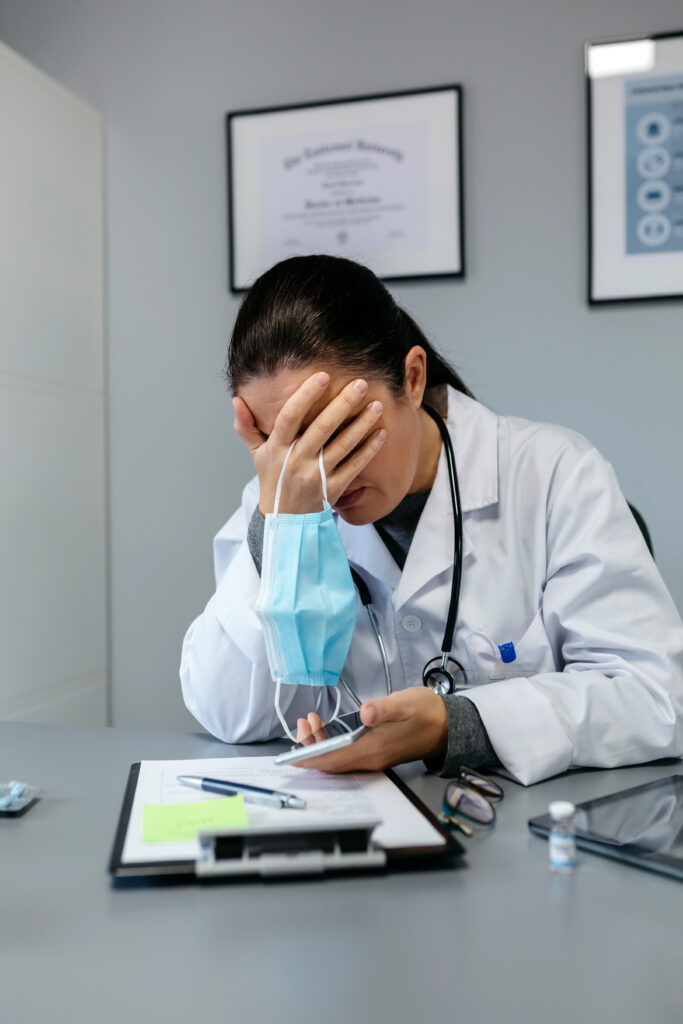
The COVID-19 pandemic has resulted in unprecedented and often devastating new circumstances for healthcare providers (HCPs), leading to an increased need for mental health prevention and early interventions efforts to support this critical workforce.
This two-hour event features:
- Research presentations about the impact of moral injury and moral distress on both Canadian and global healthcare providers
- A panel discussion with Canadian healthcare providers who have worked — and continue to work — throughout the pandemic
- A panel discussion with mental health researchers who are studying risk and mitigating factors of MI/MD in HCPs
CONTENT WARNING
During this event, we discuss examples of moral distress, moral injury, and other challenges in the work life and home life of healthcare providers during the COVID-19 pandemic. Some moments may be disturbing for you. It’s fine if you wish to stop watching at any point.
If you require wellness support, we encourage you to follow this link.
Related Links
- COVID-19 and moral injury in Canadian healthcare providers
- Predict, prevent and manage moral injuries in frontline healthcare workers and leaders facing the COVID-19 pandemic
- Associations between psychosocial stressors at work and moral injury in frontline healthcare workers and leaders facing the COVID-19 pandemic in Quebec, Canada: A cross-sectional study
Transcript
0:00:13.889,0:00:15.150
Hello and welcome.
0:00:15.150,0:00:18.740
My name is Hannah Sung and I am moderating
the symposium today.
0:00:18.740,0:00:24.210
The topic is COVID’s hidden crisis, moral
injury in healthcare providers.
0:00:24.210,0:00:27.660
This event is two hours long with a short
break in the middle.
0:00:27.660,0:00:32.230
I would like to begin by acknowledging the
land on which McMaster University is located,
0:00:32.230,0:00:36.700
which is the traditional territory of the
Haudenosaunee and Anishinaabe nations, and
0:00:36.700,0:00:40.699
within the lands protected by the Dish With
One Spoon Wampum belt.
0:00:40.699,0:00:45.500
That wampum uses the symbolism of a dish to
represent the territory and a spoon to represent
0:00:45.500,0:00:48.910
that people should share resources and only
take what they need.
0:00:48.910,0:00:54.269
Toronto, which is where I am located today,
is home to many diverse First Nations, Inuit,
0:00:54.269,0:00:58.230
and Métis people, and is covered by the Treaty
13 and the Williams Treaties.
0:00:58.230,0:01:03.019
I hope you can take a moment to consider the
treaty territory you are on and what Land
0:01:03.019,0:01:07.040
Back and stewardship of the land mean to you
and your community.
0:01:07.040,0:01:10.280
And in fact, I’d love to hear where you are
this morning.
0:01:10.280,0:01:14.660
Chat your location if you like, just drop
the name of your city or town.
0:01:14.660,0:01:17.010
It’s nice to warm up the chat that way.
0:01:17.010,0:01:23.820
The chat is a space for you today, so please
keep it respectful and on topic.
0:01:23.820,0:01:28.190
This symposium is part of a larger project
called Healthcare Salute: Thank You for Your
0:01:28.190,0:01:33.799
Service, which is funded through PHAC, the
Public Health Agency of Canada.
0:01:33.799,0:01:37.860
And Dr. Margaret McKinnon, who you’ll be meeting
in just a moment, has been working with her
0:01:37.860,0:01:42.759
team to gather evidence on the mental health
impacts of working as healthcare providers
0:01:42.759,0:01:45.329
during the pandemic.
0:01:45.329,0:01:49.360
Data has been gathered using interviews and
surveys with healthcare providers around the
0:01:49.360,0:01:53.969
country, and the researchers will be sharing
their findings today.
0:01:53.969,0:01:58.229
Several Canadian researchers are joining to
provide insight into risk and mitigating factors
0:01:58.229,0:01:59.469
on moral injury.
0:01:59.469,0:02:05.219
And you’ll also hear from healthcare providers
who describe what they’ve experienced at work.
0:02:05.219,0:02:09.860
And it goes without saying before we begin
that we are very grateful to healthcare providers
0:02:09.860,0:02:14.110
for the work they do today and every day.
0:02:14.110,0:02:18.010
So some of what you hear today may bring up
some emotions.
0:02:18.010,0:02:20.170
That’s okay.
0:02:20.170,0:02:22.380
If you need to take a break, please do.
0:02:22.380,0:02:27.660
Maybe step away from the computer, come back,
get a glass of water, take a deep breath.
0:02:27.660,0:02:33.420
There are resources that have been compiled
and that are in the chat for you.
0:02:33.420,0:02:39.220
Please take a moment to copy and paste them
into a new browser or just take a screen cap
0:02:39.220,0:02:45.510
so that you have these numbers and websites
for your use.
0:02:45.510,0:02:51.250
And with that, I would like to introduce Dr.
Margaret McKinnon to the stage.
0:02:51.250,0:02:55.080
Hello Margaret, how are you this morning?
0:02:55.080,0:02:56.080
Good, how are you?
0:02:56.080,0:02:57.080
It’s nice to see you.
0:02:57.080,0:02:58.080
Same here.
0:02:58.080,0:03:02.739
And so today the topic is moral injury and
moral distress and why it is so important
0:03:02.739,0:03:04.760
right now to understand these things.
0:03:04.760,0:03:07.200
Can we start with some definitions?
0:03:07.200,0:03:08.860
What is moral injury?
0:03:08.860,0:03:10.250
What is moral distress?
0:03:10.250,0:03:11.810
Thank you so much, Hannah.
0:03:11.810,0:03:17.030
And before we get started, like you, I’d just
like to take a moment to acknowledge the healthcare
0:03:17.030,0:03:22.620
workers across Canada and public safety personnel
who have sacrificed so much throughout their
0:03:22.620,0:03:23.620
service.
0:03:23.620,0:03:30.360
This has been a sacrifice by healthcare workers,
but also by their families who have also been
0:03:30.360,0:03:31.360
impacted.
0:03:31.360,0:03:35.670
And we very deliberately chose the term Healthcare
Salute: Thank You for Your Service for this
0:03:35.670,0:03:36.670
project.
0:03:36.670,0:03:40.820
And also we have the honour of working very
closely with the Canadian military, and we
0:03:40.820,0:03:45.849
often use the term thank you for your service
and salute: we salute your service.
0:03:45.849,0:03:50.950
And we want to salute that same service of
healthcare workers and public safety personnel
0:03:50.950,0:03:57.190
today and thank them and their families for
their service and their sacrifice.
0:03:57.190,0:04:00.840
In talking about the research today as well,
I also want to acknowledge the people who,
0:04:00.840,0:04:03.390
and the organizations, who generously funded
this research.
0:04:03.390,0:04:07.000
And so the research that we’re presenting
today is from the Trauma and Recovery Research
0:04:07.000,0:04:12.000
Unit at McMaster University, St. Joseph’s
Healthcare, Hamilton, and Homewood Research
0:04:12.000,0:04:13.000
Institute.
0:04:13.000,0:04:18.139
It was funded by, initially by a grant from
— or rather a contract from — the Centre
0:04:18.139,0:04:23.410
of Excellence on PTSD in Ottawa, which is
now the Atlas Institute, by a very generous
0:04:23.410,0:04:27.810
donation from Homewood Health to Homewood
Research Institute, by the Public Health Agency
0:04:27.810,0:04:29.580
of Canada, and by the Canadian Institutes
of Health Research.
0:04:29.580,0:04:34.610
So we just want to take a moment as well to
thank the funders who allowed us to do this
0:04:34.610,0:04:40.000
work very early on and gather the knowledge
and information necessary for the work that
0:04:40.000,0:04:41.639
we’re talking about today.
0:04:41.639,0:04:47.660
So when we think about moral injury and moral
distress, we can think back to the words of
0:04:47.660,0:04:53.720
General Roméo Dallaire when he returned home
from Rwanda and he talked about the moral
0:04:53.720,0:04:58.190
injury and moral distress that he and the
men and women who he served with experienced
0:04:58.190,0:04:59.970
in Rwanda.
0:04:59.970,0:05:04.190
And so there, there — moral injury takes
many forms, but one is the sense that one
0:05:04.190,0:05:11.199
has either engaged in or witnessed events
that violate one’s moral and ethical values.
0:05:11.199,0:05:17.750
So for General Dallaire, he talked about being
in Rwanda and being ordered to stand down
0:05:17.750,0:05:23.770
by the United Nations and not intervene during
the genocide and the slaughter that was occurring.
0:05:23.770,0:05:28.190
And that was for him and for the men and women
with whom he served, a fundamental violation
0:05:28.190,0:05:31.940
of their ethical and moral values.
0:05:31.940,0:05:35.180
In the pandemic, and the interviews that we’ve
been doing — and others across the country
0:05:35.180,0:05:38.930
have also been doing from, other research
groups that will also be here today —we’ve
0:05:38.930,0:05:45.710
heard about, for example, when healthcare
workers have had to deny parents access to
0:05:45.710,0:05:48.660
see a critically ill child because of no-visitor
policies.
0:05:48.660,0:05:54.180
We’ve heard about the proning of older adults
and turning over an older adult who really
0:05:54.180,0:05:59.740
doesn’t want care, but their substitute decision
maker has insisted upon it, and how painful
0:05:59.740,0:06:01.150
and difficult that can be.
0:06:01.150,0:06:05.900
That proning, which takes seven people—
people talk about these things that, that
0:06:05.900,0:06:10.740
had to be done in many instances during the
pandemic, but for people it was really difficult
0:06:10.740,0:06:16.240
because it touched upon or had a sense of
betrayal of their moral or their ethical values.
0:06:16.240,0:06:21.970
Or they witnessed situations that they felt
were violation of their moral or ethical values
0:06:21.970,0:06:24.250
and were powerless to intervene.
0:06:24.250,0:06:30.940
We also heard from General Dallaire when he
returned home about the betrayal that he and
0:06:30.940,0:06:35.490
the men and women he served with felt that
they had experienced, and they talked about
0:06:35.490,0:06:41.750
being ordered to stand down, and the impact
that that had on those who they were there
0:06:41.750,0:06:42.750
to protect.
0:06:42.750,0:06:47.470
So the citizens of Rwanda, and also on the
Canadian Armed Forces, where he said this
0:06:47.470,0:06:54.590
was a betrayal by an organization that had
a duty of care to people, the people of Rwanda,
0:06:54.590,0:06:57.780
and also to those who were serving within
Rwanda.
0:06:57.780,0:07:01.919
And here we’ve heard healthcare workers talk
about in this context, about for example,
0:07:01.919,0:07:06.590
being provided with very light masks at the
beginning of the pandemic.
0:07:06.590,0:07:11.840
I even saw a video where I saw nurses being
instructed to wear Kleenexes, while they transported
0:07:11.840,0:07:14.139
bodies, over their faces.
0:07:14.139,0:07:15.139
Yes.
0:07:15.139,0:07:20.840
And so, many people serving in healthcare
at the time and continuing on, have felt that
0:07:20.840,0:07:27.650
perhaps there was not enough preparedness
for a pandemic in some situations.
0:07:27.650,0:07:31.340
Also that they felt that the organizations
or individuals who they were serving with
0:07:31.340,0:07:35.949
had a duty of care to them, and they felt
that that duty of care was not met — or
0:07:35.949,0:07:39.229
to patients as well, and families throughout
the country.
0:07:39.229,0:07:42.280
And so this really is the concept of moral
injury.
0:07:42.280,0:07:49.610
So the notion that one has engaged in or witnessed
or been powerless to prevent events or incidents
0:07:49.610,0:07:55.360
that violate one’s moral and ethical values,
or that they have felt a betrayal by an individual
0:07:55.360,0:08:03.280
and organization who they feel has a duty
of care to them during the pandemic.
0:08:03.280,0:08:09.900
There’s a lot of complex context there in
terms of understanding moral injury and moral
0:08:09.900,0:08:11.720
distress.
0:08:11.720,0:08:18.430
I hear that on an individual level it’s about
a violation of your own moral code and the
0:08:18.430,0:08:20.800
stress that that entails.
0:08:20.800,0:08:27.120
And I wonder when you use the term moral injury,
can you describe how it is an injury?
0:08:27.120,0:08:29.330
Can you tell us more about that?
0:08:29.330,0:08:35.490
So, moral injury, I would say is something
that exists in itself.
0:08:35.490,0:08:40.580
It is associated with post-traumatic stress
injuries, with depression, and with anxiety.
0:08:40.580,0:08:41.849
But it’s separate.
0:08:41.849,0:08:45.160
It has a different presentation.
0:08:45.160,0:08:51.640
And when a moral injury occurs, what we often
see is an increase in — we can see increases
0:08:51.640,0:08:58.360
for example in suicidality; difficulty functioning
at home, at work, at school; we might see
0:08:58.360,0:09:03.649
an increase in symptoms of depression, anxiety,
post-traumatic stress disorder, difficulty
0:09:03.649,0:09:06.470
sleeping and insomnia, increased substance
use and abuse.
0:09:06.470,0:09:09.990
And so really this is a form of injury.
0:09:09.990,0:09:15.520
We always talk about physical injuries, but
we don’t talk as much about psychological
0:09:15.520,0:09:16.520
injuries.
0:09:16.520,0:09:20.360
And this is a psychological injury that has
occurred to an individual.
0:09:20.360,0:09:26.610
It’s resolved again of their service and their
sacrifice.
0:09:26.610,0:09:27.810
Thank you so much for that.
0:09:27.810,0:09:28.810
Margaret.
0:09:28.810,0:09:33.450
I know that we’re going to be hearing from
you again later on this morning.
0:09:33.450,0:09:38.030
First we are going to hear some findings from
your research team.
0:09:38.030,0:09:42.760
Did you have anything you wanted to add just
before we move on?
0:09:42.760,0:09:49.149
I would just again like to thank the individuals
and organizations who sponsored this research.
0:09:49.149,0:09:53.990
So again, the Public Health Agency of Canada,
the Homewood — Homewood Health Incorporated
0:09:53.990,0:09:57.810
through the generous donation to Homewood
Research Institute — Centre of Excellence
0:09:57.810,0:10:00.970
on PTSD, and of course the Canadian Institutes
of Health Research.
0:10:00.970,0:10:06.100
This work would not be possible without them,
and I think it’s work that really we need
0:10:06.100,0:10:11.500
to do in order to best support healthcare
workers, public safety personnel, and their
0:10:11.500,0:10:12.770
families over this time.
0:10:12.770,0:10:14.890
So thank you Hannah, very much.
0:10:14.890,0:10:17.140
And thank you so much for moderating this
session.
0:10:17.140,0:10:19.029
We’re really grateful.
0:10:19.029,0:10:22.740
I’m just so happy to be here and to be learning
for sure.
0:10:22.740,0:10:28.040
And so speaking of learning, we are going
to go now to a short presentation from a member
0:10:28.040,0:10:31.190
of Margaret’s research team Yuanxin Xue.
0:10:31.190,0:10:34.000
Hi everyone, thanks for having me here today.
0:10:34.000,0:10:39.720
My name is Yuanxin Xue, and I had the pleasure
to work with the Trauma and Recovery lab led
0:10:39.720,0:10:42.810
by Dr. Margaret McKinnon over the past year
and a half.
0:10:42.810,0:10:47.320
I’m really excited to be here to share some
of the results we found in a scoping review.
0:10:47.320,0:10:51.450
We started the summer of 2021 and that we
completed earlier this year.
0:10:51.450,0:10:57.000
So it’s on the potential circumstances associated
with the moral injury and moral distress in
0:10:57.000,0:10:59.880
a healthcare workers and public safety personnel.
0:10:59.880,0:11:03.410
And this is specifically during the pandemic.
0:11:03.410,0:11:07.779
So I just want to warn you, this is a fairly
short presentation, so there may be some details
0:11:07.779,0:11:14.000
on the slides that I won’t be directly speaking
to, but they’ll still be there for your reference.
0:11:14.000,0:11:19.870
So, we knew that healthcare workers and public
safety personnel were encountering many morally
0:11:19.870,0:11:23.200
and ethically challenging situations during
the pandemic.
0:11:23.200,0:11:27.360
And we really wanted to see what was out there
in the literature in terms of the circumstances
0:11:27.360,0:11:32.339
that may cause or may potentially lead to
moral injury and moral distress.
0:11:32.339,0:11:37.279
So this is the research question we used to
guide our review: What are the shared and
0:11:37.279,0:11:42.750
unique circumstances of healthcare workers
and public safety personnel during COVID globally
0:11:42.750,0:11:46.720
that are potentially associated with moral
distress and moral injury?
0:11:46.720,0:11:52.470
So here are some of the abbreviations I’ll
be using throughout the slides, and I just
0:11:52.470,0:11:56.370
want to direct your attention to the last
one there, P.M.I.D.E.
0:11:56.370,0:12:01.380
But this one stands for potentially morally
injurious or distressful event.
0:12:01.380,0:12:06.279
And we used this term to look at moral injury
and moral distress as a collective.
0:12:06.279,0:12:09.980
Our goal wasn’t really to try to delineate
between these two terms, so we thought it
0:12:09.980,0:12:18.639
would be a better idea to look at them together
and to see moral stressors more holistically.
0:12:18.639,0:12:20.540
So here’s a brief overview of our methods.
0:12:20.540,0:12:26.421
We started our search in, or the search of
our articles, in the beginning of 2020 and
0:12:26.421,0:12:27.579
we went until May 2021.
0:12:27.579,0:12:33.699
And we included any article that talked about
healthcare workers or select public safety
0:12:33.699,0:12:39.170
personnel populations in the COVID-19 context,
and they also focused on circumstances that
0:12:39.170,0:12:41.960
might lead to moral injury or moral distress.
0:12:41.960,0:12:47.150
So that’s definitely a bit of a oversimplification,
but you can find the more detailed methods
0:12:47.150,0:12:48.150
online.
0:12:48.150,0:12:53.530
And from that search, we identified approximately
1400 articles and in the very end included
0:12:53.530,0:12:54.530
57.
0:12:54.530,0:12:58.230
So before I get onto this map here, I just
wanted to say that out of the 57 articles,
0:12:58.230,0:13:01.560
all of them were primarily focused on healthcare
workers.
0:13:01.560,0:13:06.579
There was only a very small subsample of public
safety personnel in six of those articles,
0:13:06.579,0:13:09.830
but they were also aggregated with the healthcare
workers as well.
0:13:09.830,0:13:12.260
So it’s really hard to differentiate those
results.
0:13:12.260,0:13:16.170
So for the most part, the results I’ll be
talking about today, they’re primarily relevant
0:13:16.170,0:13:20.410
to healthcare workers, but that’s not to say
that they’re not relevant to public safety
0:13:20.410,0:13:23.310
personnel as well, we just need to do a bit
more research.
0:13:23.310,0:13:28.820
So this here is the world map and we have
different parts shaded in just based on the
0:13:28.820,0:13:31.959
included studies and the populations they
studied.
0:13:31.959,0:13:37.360
So you can see that the majority of articles
are focused on North America and there was
0:13:37.360,0:13:43.279
some in East Asia and South Asia, some in
Europe, and a few others across the globe
0:13:43.279,0:13:45.850
as well.
0:13:45.850,0:13:51.149
And in terms of the results we found, so after
collecting all the relevant data and coding
0:13:51.149,0:13:57.269
them, we’re able to come up with the six overarching
themes that describe the types of circumstances
0:13:57.269,0:14:01.259
associated with potentially morally injuries
or distressful events.
0:14:01.259,0:14:05.370
So the first one here, it had to do with the
risk of contracting or transmitting COVID-19.
0:14:05.370,0:14:08.290
There were 34 articles included.
0:14:08.290,0:14:13.540
And we saw that some articles spoke about
how this is particularly relevant for healthcare
0:14:13.540,0:14:17.940
workers who were more vulnerable to having
severe infection, or those that were living
0:14:17.940,0:14:19.050
with vulnerable populations.
0:14:19.050,0:14:22.699
Now, the second one here, the inability to
work on the frontlines.
0:14:22.699,0:14:27.620
This one really speaks to some of that guilt
that healthcare workers have faced when they
0:14:27.620,0:14:31.153
didn’t have the same level of risk or exposure
compared to some of their colleagues who were
0:14:31.153,0:14:32.850
on the frontlines.
0:14:32.850,0:14:37.300
And this also included people who needed to
quarantine, and then there was that additional
0:14:37.300,0:14:38.860
workload that was placed on their other colleagues.
0:14:38.860,0:14:44.529
The third one here is the provision of suboptimal
care.
0:14:44.529,0:14:48.450
And this one really just refers to healthcare
workers not being able to provide that same
0:14:48.450,0:14:51.009
level of care as they would’ve liked to.
0:14:51.009,0:14:56.360
And this was partially exacerbated by all
of the uncertainty during the pandemic, but
0:14:56.360,0:15:00.470
also by the infection control measures that
created distance between the providers and
0:15:00.470,0:15:04.870
patients, as well as the visitation policies
that made it difficult for family gatherings.
0:15:04.870,0:15:10.730
The fourth thing here, it refers to care prioritization
and resource allocation.
0:15:10.730,0:15:14.600
So this really refers to all those tough decisions
healthcare workers had to make when resources
0:15:14.600,0:15:19.089
were scarce and there was only a limited capacity
to do what they could.
0:15:19.089,0:15:21.790
This was especially tough when it came to
critical care resources.
0:15:21.790,0:15:27.529
The fifth theme here, it refers to healthcare
workers perception of that lack of support
0:15:27.529,0:15:29.310
and unfair treatment by their organization.
0:15:29.310,0:15:35.250
And so some of the ideas that I were in this
category included not having adequate benefits
0:15:35.250,0:15:39.860
or protection for the workers, as well as
the lack of communication and transparency
0:15:39.860,0:15:43.120
about the whole situation.
0:15:43.120,0:15:49.430
And the last one here, it’s the stigma, discrimination,
and abuse the healthcare workers faced.
0:15:49.430,0:15:54.180
Some of the articles included in the section
spoke to how healthcare workers, they were
0:15:54.180,0:15:58.070
viewed as virus carriers by their friends,
colleagues, and even their family.
0:15:58.070,0:16:03.060
Some experienced discrimination by their community
and others also reported acts of violence
0:16:03.060,0:16:06.800
by patients and other families.
0:16:06.800,0:16:12.149
So when we look at all these themes and the
articles that were included in each in terms
0:16:12.149,0:16:17.089
of where they’re geographically located, for
the most part, all of these themes, apart
0:16:17.089,0:16:19.959
from one, they are fairly globally spread.
0:16:19.959,0:16:25.220
And this is especially true for the risk of
contracting or transmitting COVID-19, as well
0:16:25.220,0:16:29.350
as the perceived lack of support and unfair
treatment by their organization.
0:16:29.350,0:16:34.529
So the only exception was the category of
stigma, discrimination, and abuse, where there
0:16:34.529,0:16:36.519
was a lack of articles from North America.
0:16:36.519,0:16:42.540
But this is not mean to say that this doesn’t
happen in North America, but it’s more likely
0:16:42.540,0:16:47.690
due to potential underreporting of some of
these issues in the context of moral injury
0:16:47.690,0:16:49.290
and moral distress.
0:16:49.290,0:16:52.860
And we definitely need to do more research
to get a better understanding of the severity
0:16:52.860,0:16:55.470
of those experiences and the.
0:16:55.470,0:17:00.100
So with that, that concludes the presentation
and I just want to say thank you to Dr. Margaret
0:17:00.100,0:17:04.189
McKinnon, as well as everyone who contributed
and really made this review possible.
0:17:04.189,0:17:07.090
And thank you guys so much for listening today.
0:17:07.090,0:17:11.871
It was a pleasure to speak with you all.
0:17:11.871,0:17:17.740
Thank you so much to Yuanxin who will be hearing
from in one moment.
0:17:17.740,0:17:23.300
First we’re going to hear from another presentation
from another member of this research team.
0:17:23.300,0:17:24.740
It’s from Andrea Brown.
0:17:24.740,0:17:26.520
So let’s watch.
0:17:26.520,0:17:28.250
Thank you for inviting me to speak today.
0:17:28.250,0:17:32.230
My name is Andrea Brown and I’m a research
associate in the Trauma and Recovery Research
0:17:32.230,0:17:33.880
Unit at McMaster University.
0:17:33.880,0:17:40.450
Since September of 2020, we have been collecting
information about moral injury and healthcare
0:17:40.450,0:17:41.540
providers across Canada.
0:17:41.540,0:17:46.169
And what we’re finding is that healthcare
providers are in fact experiencing moral injury
0:17:46.169,0:17:49.610
during the pandemic.
0:17:49.610,0:17:54.580
Moral injury has been called the signature
wound of service, although this was originally
0:17:54.580,0:17:59.169
brought forward for military members, we also
believe that it applies to our healthcare
0:17:59.169,0:18:00.980
providers.
0:18:00.980,0:18:07.400
In our very first webinar in the Healthcare
Salute series, Kim Ritchie and Andrea D’Alessandro-Lowe
0:18:07.400,0:18:13.140
gave some information about the types of events
that healthcare providers have identified
0:18:13.140,0:18:17.030
as morally injurious or morally distressing.
0:18:17.030,0:18:19.740
These include witnessing patients dying alone.
0:18:19.740,0:18:25.039
At one point, during the pandemic, family
members weren’t allowed to go and and have
0:18:25.039,0:18:27.570
end of lifetime with their loved ones.
0:18:27.570,0:18:31.600
And during this time, healthcare providers
had to watch their patients dying alone.
0:18:31.600,0:18:35.900
And this spanned the age ranges of very old
to very young.
0:18:35.900,0:18:41.940
Also providing invasive care, which is perceived
as futile and prolongs the suffering of their
0:18:41.940,0:18:42.940
patients.
0:18:42.940,0:18:47.770
Increasing workload and decreasing staff,
which is an something that’s impacting our
0:18:47.770,0:18:50.330
healthcare providers even today.
0:18:50.330,0:18:57.360
Bullying, violence and divided opinions as
well as the disconnect between frontline staff
0:18:57.360,0:19:00.640
and their organization.
0:19:00.640,0:19:05.549
So we know the types of events that are being
identified as morally injurious or morally
0:19:05.549,0:19:10.930
distressing by healthcare providers, but we’re
also wondering what are the impacts.
0:19:10.930,0:19:18.549
In particular, we’re wondering about post-traumatic
stress, depression, anxiety, stress, dissociation,
0:19:18.549,0:19:19.640
substance use, and resilience.
0:19:19.640,0:19:23.620
Are these things that are also impacting our
healthcare providers?
0:19:23.620,0:19:31.659
So in order to understand this better, we
have had a survey, or we had a survey that
0:19:31.659,0:19:37.539
was open from September of 2020 until September
of 2022, and it was open to healthcare providers
0:19:37.539,0:19:39.560
across Canada to complete.
0:19:39.560,0:19:43.710
The bulk of our participants were nurses and
respiratory therapists, but we also had many
0:19:43.710,0:19:50.160
other healthcare providers complete, including
occupational therapists, physicians, those
0:19:50.160,0:19:52.940
in dentistry, long-term care and mental health.
0:19:52.940,0:20:00.560
And in total, we had nearly 700 people complete
the survey or partially complete the survey.
0:20:00.560,0:20:03.890
Near 80% of our participants identified as
being female.
0:20:03.890,0:20:07.580
The bulk were from Ontario living and practicing.
0:20:07.580,0:20:12.049
We also had nearly 10% from Alberta and British
Columbia.
0:20:12.049,0:20:16.970
We did have representation from across the
provinces, although we didn’t have representation
0:20:16.970,0:20:23.110
from the territories, and nearly 70% of our
participants identified as having European
0:20:23.110,0:20:26.390
ancestry.
0:20:26.390,0:20:30.010
The first question we really wanted to know
is how many of our participants said that
0:20:30.010,0:20:34.659
they were experiencing these events or these
situations that they would define as morally
0:20:34.659,0:20:35.659
injurious.
0:20:35.659,0:20:41.730
So we asked them a question asking if they
had been exposed to three types of events
0:20:41.730,0:20:45.010
that goes against their core, their moral
codes or values.
0:20:45.010,0:20:50.409
So these are events in which they did something
or didn’t do something that went against their
0:20:50.409,0:20:56.049
moral code, they witnessed somebody else doing
something or not doing something that went
0:20:56.049,0:21:01.500
against their moral code and then being directly
impacted by something that somebody else did
0:21:01.500,0:21:04.990
or didn’t do that went against the moral code
or their values.
0:21:04.990,0:21:11.039
So what we found is that 70% of our participants
were exposed to these types of events that
0:21:11.039,0:21:17.690
went against their moral code or their values,
and 67% of our participants said that they
0:21:17.690,0:21:19.620
experienced these events in 2021.
0:21:19.620,0:21:28.179
And 72% of our participants in 2022 said that
they had experienced these events this year,
0:21:28.179,0:21:31.600
and that was between January and September.
0:21:31.600,0:21:36.770
So we know the types of events that are being
defined as morally injurious, and we know
0:21:36.770,0:21:41.890
that two-thirds of our healthcare population
are experiencing these types of events.
0:21:41.890,0:21:46.440
So then we wanted to know how is it impacting
them?
0:21:46.440,0:21:52.960
So we asked questions in our survey, and what
we found was that those who perceived a greater
0:21:52.960,0:22:03.789
moral injury also experienced greater rates
of depression, anxiety, stress, post-traumatic
0:22:03.789,0:22:06.679
stress, and dissociation.
0:22:06.679,0:22:12.620
These are at a statistically significant level,
but we also found that those who had greater
0:22:12.620,0:22:18.080
perceived moral injuries also used more substances
in order to try and cope.
0:22:18.080,0:22:24.080
So this includes increasing alcohol use, cannabis
use, and other recreational drugs.
0:22:24.080,0:22:29.720
Although this wasn’t statistically significant,
there was a positive correlation between the
0:22:29.720,0:22:30.720
two.
0:22:30.720,0:22:36.490
And what we also found is that those who had
perceived greater moral injury also had decreased
0:22:36.490,0:22:37.490
resilience.
0:22:37.490,0:22:43.640
So this is the feelings that they could cope
with the stresses and that they could bounce
0:22:43.640,0:22:45.059
back with the stresses.
0:22:45.059,0:22:51.110
So we know that what the morally injurious
events are, we know that two-thirds at least
0:22:51.110,0:22:54.890
of our healthcare population are experiencing
these events, and we know that it’s impacting
0:22:54.890,0:23:01.550
their mental health, their coping ability,
and their ability to bounce back.
0:23:01.550,0:23:06.309
So together with our collaborators, we have
created some recommendations for healthcare
0:23:06.309,0:23:11.679
organizations and leaders, and it begins with
listening and understanding healthcare providers’
0:23:11.679,0:23:16.990
experiences and the impact these experiences
have had on healthcare providers and their
0:23:16.990,0:23:21.870
family, because the impacts go home with them.
0:23:21.870,0:23:26.910
Asking healthcare providers questions about
what they need to perform their roles and
0:23:26.910,0:23:33.190
improve their mental health, because healthcare
providers know what they need more than anybody.
0:23:33.190,0:23:38.289
And then providing access to appropriate supports
for healthcare providers.
0:23:38.289,0:23:44.610
So taking what you’ve learned when you’re
listening to their experiences and understanding
0:23:44.610,0:23:48.450
what it is that they need, and then providing
them with those supports.
0:23:48.450,0:23:55.150
The supervisors and the management in these
organizations are also under a lot of stress.
0:23:55.150,0:24:00.190
They have to balance the needs of the healthcare
providers and the organizations to make sure
0:24:00.190,0:24:04.160
that the services are being provided for our
population.
0:24:04.160,0:24:09.049
So another recommendation we made is to provide
supervisors and management with resources
0:24:09.049,0:24:13.330
and training to support healthcare providers’
mental health.
0:24:13.330,0:24:20.110
And finally, we recommend to establish evidence-based
policies to guide ethically difficult decisions.
0:24:20.110,0:24:25.159
While on the job, healthcare providers have
to make life-and-death decisions.
0:24:25.159,0:24:30.860
And they said it would be helpful if they
had policies to help guide these decisions
0:24:30.860,0:24:35.520
and that these policies were based in evidence.
0:24:35.520,0:24:41.020
So to summarize my very short presentation
today, we know that healthcare providers are
0:24:41.020,0:24:46.140
experiencing moral injury, and we also know
the types of events that they are saying are
0:24:46.140,0:24:47.860
morally injurious.
0:24:47.860,0:24:52.770
We also know that these moral injuries are
impacting their mental health, their ability
0:24:52.770,0:24:55.640
to bounce back, and substance use.
0:24:55.640,0:25:02.480
So what we are going to do is to continue
to conduct research to identify interventions
0:25:02.480,0:25:09.070
and to identify the long-term impacts of these
moral injuries.
0:25:09.070,0:25:11.320
Thank you very much.
0:25:11.320,0:25:12.390
Thank you so much, Andrea.
0:25:12.390,0:25:17.390
And I have a feeling that there were probably
many people in this webinar who are nodding
0:25:17.390,0:25:23.169
along to the observations and the details
and the recommendations that you just shared
0:25:23.169,0:25:24.279
with us.
0:25:24.279,0:25:34.210
So I would like to invite Yuanxin and Andrea
to join me for a quick debrief of your presentations.
0:25:34.210,0:25:39.210
Your presentations were filled with detail,
and I would like to just go very big picture
0:25:39.210,0:25:40.780
if I may.
0:25:40.780,0:25:47.330
And first I’ll ask you, Yuanxin: you showed
us the map of all the various places from
0:25:47.330,0:25:48.870
which you drew your research.
0:25:48.870,0:25:54.830
Did you find important similarities between
your findings globally and the data in Canada?
0:25:54.830,0:25:55.830
Yeah.
0:25:55.830,0:25:57.410
No, no, for sure.
0:25:57.410,0:25:58.410
And thank you for that question.
0:25:58.410,0:26:01.080
I think that was actually a big part of why
we started the review.
0:26:01.080,0:26:06.870
We wanted to see if what we’re seeing in Canada
was really happening across the globe as well.
0:26:06.870,0:26:10.580
And although most of the articles were more
the based in North America, I think we did
0:26:10.580,0:26:14.030
get a glimpse of what it does look like globally.
0:26:14.030,0:26:19.279
And I think like when you look at the themes
we found and the other information that we
0:26:19.279,0:26:23.750
gathered on Canadian healthcare workers through
the interviews and the surveys they’re basically
0:26:23.750,0:26:28.060
saying the same thing, but just they’re just
organized a little bit differently.
0:26:28.060,0:26:33.190
And I think two of the really big similarities,
there’s probably anything that’s related to
0:26:33.190,0:26:38.330
patients and not being able to provide the
optimal care that they used to be — whether
0:26:38.330,0:26:45.049
it be not having, having patients that had
to die alone because of visitor policies or
0:26:45.049,0:26:51.169
other limitations to work because of increased
workloads or changing protocols, or simply
0:26:51.169,0:26:57.100
just witnessing like patients who were receiving
care that healthcare workers may have felt
0:26:57.100,0:26:58.480
was futile.
0:26:58.480,0:27:02.380
I think that was definitely a big similarity
between what we see here, as well as in the
0:27:02.380,0:27:03.380
review.
0:27:03.380,0:27:10.440
And I would say another big area was had to
do with the organizations, and that just perceived
0:27:10.440,0:27:14.010
a lack of support or sometimes even betrayal.
0:27:14.010,0:27:20.850
The healthcare workers felt when there was
inadequate PPE, inadequate staffing, and just
0:27:20.850,0:27:27.880
that disconnect that sometimes there was between
the frontline workers and their organization.
0:27:27.880,0:27:36.519
Well, I find that so interesting that you
found those key similarities because, as someone
0:27:36.519,0:27:40.720
who doesn’t work in healthcare, I would think
that depending on your region, depending on
0:27:40.720,0:27:46.149
the type of healthcare system, that there
would be some real specificity about the work
0:27:46.149,0:27:47.149
that happens.
0:27:47.149,0:27:53.309
But in fact, there were certain experiences
that healthcare workers had just across the
0:27:53.309,0:27:54.620
board during the pandemic.
0:27:54.620,0:27:56.520
Mm-hmm, for sure.
0:27:56.520,0:28:00.070
I think like when you look at big picture,
I think it’s pretty much, you’re looking at
0:28:00.070,0:28:01.070
the same things.
0:28:01.070,0:28:05.880
But maybe if you like zoom into Canada or
different parts of the world, the severity
0:28:05.880,0:28:09.171
or extent to certain experiences, that that
might differ.
0:28:09.171,0:28:14.090
But I think for the most part we’re seeing
that healthcare workers, they were experiencing
0:28:14.090,0:28:18.120
moral injury, they were experiencing moral
distress and there’s definitely a lot that
0:28:18.120,0:28:19.630
can be done there.
0:28:19.630,0:28:20.780
Mm-hmm.
0:28:20.780,0:28:22.440
Thank you Yuanxin.
0:28:22.440,0:28:23.760
I would like to move over to —
0:28:23.760,0:28:25.159
Can I just add on to that?
0:28:25.159,0:28:26.159
Andrea, please do.
0:28:26.159,0:28:27.159
Yeah.
0:28:27.159,0:28:28.159
Okay.
0:28:28.159,0:28:31.880
So during Yuanxin’s presentation, he said
that the one area that wasn’t as supported
0:28:31.880,0:28:38.080
in North America was the stigma, discrimination,
and abuse, but I think that might be because
0:28:38.080,0:28:40.260
of when those publications took place.
0:28:40.260,0:28:44.620
Cause our research is actually finding that
in the last year, that is a moral injury that
0:28:44.620,0:28:48.240
has come up more and more in our conversations
with healthcare providers.
0:28:48.240,0:28:53.650
So it could just be that the research ended
and was published towards the end of 2021.
0:28:53.650,0:28:56.730
So that means it was submitted before that.
0:28:56.730,0:29:00.200
So in the last year it actually has risen.
0:29:00.200,0:29:01.200
Yes.
0:29:01.200,0:29:05.269
It’s interesting because in your presentation
you said, Andrea, that you were looking at
0:29:05.269,0:29:12.059
research or you, you, your team was conducting
surveys that go all the way up to just a couple
0:29:12.059,0:29:14.940
of months ago, until September 2022?
0:29:14.940,0:29:17.390
The end of September, right.
0:29:17.390,0:29:18.390
Yeah.
0:29:18.390,0:29:23.330
So I would love to ask you, Andrea, again,
very big picture, why do you think it’s important
0:29:23.330,0:29:28.230
to understand how moral injury specifically
is related to mental health when it comes
0:29:28.230,0:29:29.710
to healthcare providers?
0:29:29.710,0:29:37.340
I think the big thing, Hannah, is that understanding
the impact of moral injury on healthcare providers
0:29:37.340,0:29:41.860
will help us to provide them with the supports
that they need and what types of supports
0:29:41.860,0:29:43.549
that they need to have.
0:29:43.549,0:29:46.230
Healthcare providers play a vital role in
our society.
0:29:46.230,0:29:50.179
And it’s one of the things that Canadians
are always so proud of, is our healthcare
0:29:50.179,0:29:51.340
system.
0:29:51.340,0:29:55.529
Our healthcare providers, who have always
made life-and-death types of decisions, and
0:29:55.529,0:30:01.080
have always been in these types of situations,
something about COVID-19 is different, and
0:30:01.080,0:30:02.970
it’s intensified everything.
0:30:02.970,0:30:10.120
And so we now know that they’re facing moral
injuries, and we know how it’s impacting them.
0:30:10.120,0:30:17.289
So we as society, at the government level
and at the organizational, understanding this
0:30:17.289,0:30:23.050
can start to implement the behaviours and
the skills and support for our healthcare
0:30:23.050,0:30:27.700
providers to help them while they’re helping
us.
0:30:27.700,0:30:29.590
Mm-hmm.
0:30:29.590,0:30:36.200
And I’m glad to see that there are some questions
that are coming through the chat.
0:30:36.200,0:30:43.649
So I will say that there are probably too
many to get to them all, but please keep them
0:30:43.649,0:30:45.960
coming and I will get to as many as I can.
0:30:45.960,0:30:49.440
So I’m just going to choose one here for you
both, Yuanxin and Andrea.
0:30:49.440,0:30:55.450
Karen is asking, when gender-based analysis
was applied to your research, were there any
0:30:55.450,0:31:03.809
important variations and findings based on
specific occupation and/or sex and gender
0:31:03.809,0:31:05.929
of the healthcare provider?
0:31:05.929,0:31:09.080
Would either of you like to speak to that?
0:31:09.080,0:31:16.360
At this time, I have not run the analyses
on the gender based analysis.
0:31:16.360,0:31:21.309
But I would reiterate that 80% of our population
identified as being female.
0:31:21.309,0:31:25.669
So it’ll be a small percentage that identify
as male or non-binary.
0:31:25.669,0:31:31.109
Thank you.
0:31:31.109,0:31:35.090
And I will ask one more question.
0:31:35.090,0:31:40.970
What are the next steps in terms of interventions,
any suggestions and or recommendations?
0:31:40.970,0:31:45.149
I know, Andrea, that there were several in
your presentation.
0:31:45.149,0:31:48.510
Maybe you can go into some of them in detail.
0:31:48.510,0:31:49.510
Sure.
0:31:49.510,0:31:55.139
So, one of the things that’s come out of our
research is that we’ve made some recommendation,
0:31:55.139,0:32:02.150
and I know that Sangita has put a link to
these recommendations within the, in the chat.
0:32:02.150,0:32:06.460
In addition, with the funding that we’re receiving
from the Public Health Agency of Canada, we
0:32:06.460,0:32:11.070
are creating some psychoeducational programs
that will be available online.
0:32:11.070,0:32:18.179
It includes some training for trauma-informed
care for, for not — it can be used by healthcare
0:32:18.179,0:32:23.779
providers in their work, but it can also be
for people who are supporting healthcare providers
0:32:23.779,0:32:29.580
and understanding that everybody has traumas
and when we’re working together, these traumas
0:32:29.580,0:32:31.020
are impacting people regardless.
0:32:31.020,0:32:37.269
So when you’re dealing with somebody, realize
that they’re, they might not always be in
0:32:37.269,0:32:40.860
the same situation that you are because of
what’s happened in the past or what’s ongoing
0:32:40.860,0:32:48.269
at work, or also creating with the University
of Alberta some psychoed programs, online
0:32:48.269,0:32:50.330
programs on what is moral injury.
0:32:50.330,0:32:56.019
And then we’ve also created one on PTSD stress.
0:32:56.019,0:32:59.899
And that will help people to understand, let’s
say that you’re a healthcare provider and
0:32:59.899,0:33:03.090
you really don’t understand why you’re not
sleeping well.
0:33:03.090,0:33:07.760
And I’m sure that healthcare providers do
understand this, but it’ll help to go in and
0:33:07.760,0:33:12.490
say, PTSD and stress and moral injury, this
is how it affects your body and this is why
0:33:12.490,0:33:13.970
you’re feeling this way.
0:33:13.970,0:33:18.330
And we will also connect you with some some
other information that you have.
0:33:18.330,0:33:26.429
And there are also supports available online
that we will connect you with.
0:33:26.429,0:33:34.289
So it sounds like the experiences that healthcare
providers may be having, it’s good to have
0:33:34.289,0:33:42.890
the language and the backup and the evidence
to show that healthcare providers need help,
0:33:42.890,0:33:46.679
and that these injuries affect the ability
to do the job?
0:33:46.679,0:33:47.679
Right.
0:33:47.679,0:33:50.760
And remembering that healthcare providers
are helpers.
0:33:50.760,0:33:56.809
They’re always helpers, and they often put
themselves lowest on their list of who to
0:33:56.809,0:33:58.590
take care of themselves.
0:33:58.590,0:34:03.700
But it shouldn’t just be on healthcare providers
to take care of themselves.
0:34:03.700,0:34:07.260
We as a society need to do what we can to
support our healthcare providers.
0:34:07.260,0:34:13.550
The government needs to put in the laws and
the regulations to support our healthcare
0:34:13.550,0:34:15.580
providers, and the organizations need to do
that too.
0:34:15.580,0:34:20.220
So let’s take the focus off the healthcare
providers taking care of their mental health,
0:34:20.220,0:34:23.290
and let’s put it on everybody to support our
healthcare providers.
0:34:23.290,0:34:24.290
Absolutely.
0:34:24.290,0:34:30.500
Well, Andrea and Yuanxin, thank you so much
for your research and your presentations.
0:34:30.500,0:34:32.000
I really appreciate it.
0:34:32.000,0:34:33.940
Thank you, Hannah.
0:34:33.940,0:34:35.240
Thank you.
0:34:35.240,0:34:36.540
Thank you.
0:34:36.540,0:34:43.859
And while we are speaking about healthcare
providers, why don’t we speak to healthcare
0:34:43.859,0:34:44.859
providers?
0:34:44.859,0:34:49.599
We have a panel of three people who have very
generously given their time and are about
0:34:49.599,0:34:51.919
to share their experiences with us.
0:34:51.919,0:34:54.820
I’d like to quickly introduce you to them.
0:34:54.820,0:34:58.960
Michele Johnson, if you could join, Krissha
Fortuna.
0:34:58.960,0:35:00.790
Jennifer Kwan.
0:35:00.790,0:35:02.339
Michele and Krissha are nurses.
0:35:02.339,0:35:04.160
Jennifer is a family doctor.
0:35:04.160,0:35:09.349
And if you’re on Twitter, if you were on Twitter
during the pandemic, you know Jennifer has
0:35:09.349,0:35:16.140
provided a lot of information there for laypeople
such as myself to understand COVID data.
0:35:16.140,0:35:23.329
So I want to ask all three of you about what
you’re hearing today about moral injury and
0:35:23.329,0:35:29.260
moral distress and whether these definitions
in these observations speak to you when you
0:35:29.260,0:35:31.030
think about your day-to-day work.
0:35:31.030,0:35:38.020
But first, can I ask you just very quickly
in 10 seconds to tell us what is your job
0:35:38.020,0:35:41.050
and what is your favourite thing about your
work.
0:35:41.050,0:35:43.880
Maybe Michelle, I’ll start with you.
0:35:43.880,0:35:45.760
Okay.
0:35:45.760,0:35:50.260
So I’m a nurse of 32 years in a hospital in
downtown Toronto.
0:35:50.260,0:35:53.360
And there’s three things I really love about
my job.
0:35:53.360,0:36:02.190
It’s this kind of collection of this science,
hands-on critical thinking and this empathetic
0:36:02.190,0:36:08.500
opportunity to meet with a stranger, a stranger
in distress, who I can reach out with my heart
0:36:08.500,0:36:12.460
and reach theirs and have a moment that’s
like — it’s an incredible privilege to be
0:36:12.460,0:36:13.530
able to do that.
0:36:13.530,0:36:20.569
And the other thing is this kind of incredible
support I get in my whole life, all aspects
0:36:20.569,0:36:22.599
of my life, that I get from my colleagues.
0:36:22.599,0:36:29.260
Like, working with people who are caregivers
is an incredible privilege, because we care
0:36:29.260,0:36:35.470
for each other in the same way we care for
the public and people we’ve never met, we
0:36:35.470,0:36:39.829
care deeply for each other — and that’s
a pretty wonderful job.
0:36:39.829,0:36:42.800
I love that description.
0:36:42.800,0:36:43.870
Thank you so much.
0:36:43.870,0:36:48.359
And I’ll also just mention, Michele, that
I think your microphone is rubbing on a little
0:36:48.359,0:36:49.359
something.
0:36:49.359,0:36:51.490
I don’t know if you want to just — yeah,
check that out.
0:36:51.490,0:36:55.819
But you sound great and maybe I’ll go to Krissha
now.
0:36:55.819,0:37:07.430
Can you tell us about your job and what you
love about it?
0:37:07.430,0:37:10.290
Krissha is not here at the moment.
0:37:10.290,0:37:16.890
I’m sorry, I introduced Krissha, but my view
of the Zoom is very complicated, so I could
0:37:16.890,0:37:20.210
not see that she’s actually not here at the
moment.
0:37:20.210,0:37:21.410
She is here!
0:37:21.410,0:37:28.160
As you can see from the chat, you have to
have a moment like this in a Zoom.
0:37:28.160,0:37:38.000
I’m not sure if we can get Mike to help out
with bringing Krissha into the panel so that
0:37:38.000,0:37:40.830
Krissha can speak with us.
0:37:40.830,0:37:43.960
But maybe for now, I’ll just go to Jennifer.
0:37:43.960,0:37:48.359
Can you tell us a little bit about your job
and your favourite thing about it?
0:37:48.359,0:37:52.570
Thanks Hannah, and thanks everyone for joining
us today.
0:37:52.570,0:37:55.560
I’m a family doctor in Burlington.
0:37:55.560,0:37:56.580
I do love my job.
0:37:56.580,0:37:58.020
I love my patients.
0:37:58.020,0:38:04.050
It is such a privilege to care for people
and their families and develop these long-term
0:38:04.050,0:38:07.490
relationships and get to know them over time.
0:38:07.490,0:38:11.500
It’s both rewarding and heartbreaking cause
sometimes we do see things happen to people,
0:38:11.500,0:38:18.570
but it’s such a privilege to be there to help
fix things that we can fix and to hold people’s
0:38:18.570,0:38:23.859
hands like figuratively when they are going
through illnesses and help people with their
0:38:23.859,0:38:24.859
health over time.
0:38:24.859,0:38:31.830
So I really do love my job and despite some
of the moral distress that we experience,
0:38:31.830,0:38:36.500
it is still a very — a great honour to be
a family doctor.
0:38:36.500,0:38:39.010
Thank you, Jennifer.
0:38:39.010,0:38:41.829
And Krissha is joining us now.
0:38:41.829,0:38:47.290
I would love for you to tell us in 10 seconds
about your job and what you love about it.
0:38:47.290,0:38:49.270
Hi, everybody.
0:38:49.270,0:38:52.230
Sorry about that.
0:38:52.230,0:38:57.810
What I love about my job is getting up to
see patients every day, helping those who
0:38:57.810,0:39:02.040
need help, who brighten.
0:39:02.040,0:39:07.670
They might need something like a flu shot
and then it will change their day.
0:39:07.670,0:39:14.950
It’s about touching, it’s about speaking in
to your patients and really connecting with
0:39:14.950,0:39:18.560
them in some ways you can to just help.
0:39:18.560,0:39:24.740
I don’t know, it’s just always an innate feeling
towards — in my line of work, it’s just,
0:39:24.740,0:39:30.619
I’ve always loved helping and I felt like
I was born, I was put in this world for the
0:39:30.619,0:39:34.470
purpose of helping somebody.
0:39:34.470,0:39:40.089
And it’s just interacting with people every
day and making a difference.
0:39:40.089,0:39:47.329
That’s how I believe how I was put in this
world, is to help people day in and day out,
0:39:47.329,0:39:48.810
no matter what.
0:39:48.810,0:39:50.690
Thank you.
0:39:50.690,0:39:51.690
Krissha.
0:39:51.690,0:39:56.829
And I know that you are a nurse and that you
work with people who are, I believe newcomers
0:39:56.829,0:39:58.670
to Canada, at the moment.
0:39:58.670,0:39:59.670
Yes.
0:39:59.670,0:40:00.670
That’s your work, correct?
0:40:00.670,0:40:01.670
Yeah.
0:40:01.670,0:40:05.210
I currently work with newcomers and refugees
coming into Canada.
0:40:05.210,0:40:16.339
I provide mostly primary care, help them go
over, like helping them with resources and
0:40:16.339,0:40:22.680
working through a lot of barriers and really
advocating for patients because how come this
0:40:22.680,0:40:28.530
patient can’t get their, what they need in
order for them to be healthy, however these
0:40:28.530,0:40:36.350
people can, and what I’ve noticed is there’s
a lot of racism involved, and there’s just
0:40:36.350,0:40:40.280
a lot of barriers for patients, especially
coming into Canada.
0:40:40.280,0:40:48.960
And myself as an immigrant, I know exactly
how I transitioned over here and how challenging
0:40:48.960,0:40:50.030
it was.
0:40:50.030,0:40:57.020
And oftentimes that’s how I’ve been connecting
and able to empathize with patients like that,
0:40:57.020,0:40:59.410
because they’re also struggling.
0:40:59.410,0:41:06.100
And then I think that’s why I have chosen
this field, is because in some ways I’m doing
0:41:06.100,0:41:09.810
more than just cleaning up a wound or whatnot.
0:41:09.810,0:41:15.599
I’m actually doing something for them for
their future.
0:41:15.599,0:41:24.609
And it, it strikes me as you’re speaking that
you work with people who are in a vulnerable
0:41:24.609,0:41:28.109
situation because they’re new to the country
and they face many barriers.
0:41:28.109,0:41:33.060
But I guess all healthcare workers come in
contact with people who are in a vulnerable
0:41:33.060,0:41:36.530
moment because they need your help.
0:41:36.530,0:41:41.770
And Krissha, if I may start with you, in terms
of experiences throughout the pandemic and
0:41:41.770,0:41:48.160
doing your work, earlier in the pandemic,
you were working in long-term care, and I
0:41:48.160,0:41:54.109
would like to know what did it feel like at
first to be managing your nursing staff, especially
0:41:54.109,0:42:00.500
when it came to outbreaks of COVID in the
facility?
0:42:00.500,0:42:08.760
So while I was working in long-term care,
I think that all of us we were all quite scared.
0:42:08.760,0:42:18.800
For us, it was kind of an invisible dooming
cloud coming in and you know, and soon as
0:42:18.800,0:42:22.470
you know it, you just get it and then it spreads
like wildfire.
0:42:22.470,0:42:31.500
So for us, it was really important for me
to ensure that staff are well protected and
0:42:31.500,0:42:38.430
they always, because you have to think about
it, they have people to come home to.
0:42:38.430,0:42:45.619
They have family, loved ones, children, grandparents,
and these are the people who rely on them.
0:42:45.619,0:42:49.400
There’s a reason why they come out and do
this job every day.
0:42:49.400,0:42:59.200
So for me, I’ve had one experience where I
had to practically raise my voice at the staff
0:42:59.200,0:43:00.349
because we were in an outbreak.
0:43:00.349,0:43:06.079
And in an outbreak situation, you really need
to be considerate and you need to be very
0:43:06.079,0:43:13.160
cautious and you need to be on your high alert
because at that time, we didn’t know what
0:43:13.160,0:43:14.160
COVID was.
0:43:14.160,0:43:19.900
We didn’t have all these informations and
how widespread it could be and how it travels
0:43:19.900,0:43:25.190
through airborne and what kind of protections
do we need.
0:43:25.190,0:43:29.650
So for me, I had to stand up for them, because
I had to tell them, “Listen, you know
0:43:29.650,0:43:30.839
what?
0:43:30.839,0:43:34.099
I need you guys to protect each other.
0:43:34.099,0:43:38.030
This is the only way we really can come out
of this.
0:43:38.030,0:43:39.310
You look out for me.
0:43:39.310,0:43:44.599
You look out for her, and you look out for
him, or you look out for your next teammate.
0:43:44.599,0:43:48.359
That is what it is all about.”
0:43:48.359,0:43:52.600
And I think I was reprimanded for the fact
that I shouldn’t be yelling, I shouldn’t be
0:43:52.600,0:44:00.510
raising my voice at staff, but I thought at
that time I was being honest and I really
0:44:00.510,0:44:07.950
laid out the reality that it could be any
of us who will get sick, and then God forbid
0:44:07.950,0:44:09.510
it spreads to other family members.
0:44:09.510,0:44:15.000
Like my dad was a diabetic — or is a diabetic.
0:44:15.000,0:44:16.800
I was very scared.
0:44:16.800,0:44:17.800
Yeah.
0:44:17.800,0:44:24.270
So that’s how some people might not like my
approach, but I felt that I had to make that
0:44:24.270,0:44:29.400
very clear, that safety was very important.
0:44:29.400,0:44:34.020
I can definitely hear that emotions were running
high because when you say you raised your
0:44:34.020,0:44:38.270
voice, you were stretched to that point where
you needed to do that.
0:44:38.270,0:44:42.920
Michele, I would like to turn to you for a
moment because you were also a nurse.
0:44:42.920,0:44:47.240
And you mentioned that you have been in nursing
for 32 years.
0:44:47.240,0:44:52.590
I feel like if you’ve been doing anything
for 32 years, you’ve probably seen it all.
0:44:52.590,0:44:55.880
But COVID was unprecedented, as we know.
0:44:55.880,0:45:00.740
Were there any firsts that you witnessed at
work during the pandemic?
0:45:00.740,0:45:01.740
Yeah.
0:45:01.740,0:45:03.220
Thanks Hannah.
0:45:03.220,0:45:05.790
There certainly were.
0:45:05.790,0:45:11.010
And just to start out with, I want to just
say thank you so much to the researchers who’ve
0:45:11.010,0:45:15.190
done this work, it’s actually touched my heart
so, so deeply.
0:45:15.190,0:45:24.250
I feel a little, it’s, it’s — I’m really
touched to, to have what I’ve experienced
0:45:24.250,0:45:31.930
and the emotions that we as nurses carry,
to have it received so wholesomely by the
0:45:31.930,0:45:35.210
researchers and reflected back, has actually
really touched my heart.
0:45:35.210,0:45:37.319
And I’m a little bit like, Whew!
0:45:37.319,0:45:48.520
This is kind of exciting to realize that all
that we have done is being so validated, and
0:45:48.520,0:45:49.520
that’s really wonderful.
0:45:49.520,0:45:50.599
So thank you for that.
0:45:50.599,0:45:57.800
And what I would like to say is what I saw
for the first time was sort of the impact
0:45:57.800,0:46:04.660
of this moral injury and moral distress and
the sort of way that COVID tipped things.
0:46:04.660,0:46:12.740
When when COVID arrived, we didn’t realize
how deeply us nurses depend on each other.
0:46:12.740,0:46:15.410
We are a resilient collective.
0:46:15.410,0:46:21.930
We are, we are a network of caregivers who
care for each other and care for our patients.
0:46:21.930,0:46:26.530
And it’s a real — I’m doing this with my
hands cause it’s a way to articulate how we
0:46:26.530,0:46:30.849
are — we’re greater than the sum of our
parts when we are together.
0:46:30.849,0:46:37.079
And when COVID came, they gave us these flimsy
little blue surgical masks and the only work
0:46:37.079,0:46:40.470
if we all wear them and we stay six feet apart.
0:46:40.470,0:46:49.490
And that imperative to isolate left us alone
and our distresses became individualized.
0:46:49.490,0:46:52.830
Prior to this, we had always come together.
0:46:52.830,0:46:58.460
I could find a colleague and say, “Hey,”
and suddenly we were individualized.
0:46:58.460,0:47:00.770
We weren’t a collective, we weren’t together.
0:47:00.770,0:47:05.780
When I experienced what any of us experienced,
the fear, the anxiety, the sorrows, when we
0:47:05.780,0:47:12.550
were in a situation of overwhelm, we were
alone with that feeling.
0:47:12.550,0:47:17.540
And I had never before seen nurses breaking
down, isolated.
0:47:17.540,0:47:19.650
We’ve all cried in our shifts.
0:47:19.650,0:47:28.810
That’s — but to have to find nurses sobbing
in utility rooms and in quiet corners, it
0:47:28.810,0:47:34.730
stood in a stark contrast to SARS, which came
20 years ago.
0:47:34.730,0:47:38.550
When it came, we were all rapidly given N95
masks in the hospital.
0:47:38.550,0:47:42.841
And the whole city was scared of us, but we
knew we were safe cause we had our N95 masks
0:47:42.841,0:47:47.810
and we knew they would keep us safe and we
were able to gather and we were able to support
0:47:47.810,0:47:48.810
each other.
0:47:48.810,0:47:54.580
And the sense of betrayal that I feel because
we’ve been denied proper PPE — because it
0:47:54.580,0:48:01.609
was, here’s your blue mask, stay apart — it
has fractured this incredible network that
0:48:01.609,0:48:05.470
nurses depend on professionally and personally.
0:48:05.470,0:48:11.640
We come to work for 12 hours and we support
each other so that we can also go home and
0:48:11.640,0:48:15.690
still be as good of people as we can be.
0:48:15.690,0:48:21.330
And I personally feel, I’m quoting Margaret,
I wrote some of her words down, like a guilt
0:48:21.330,0:48:26.680
and shame in the difficulties of, and the
moral distress of our failure to our collective
0:48:26.680,0:48:33.330
selves as nurses and allied health professionals,
including doctors, in our stuff, and there’s
0:48:33.330,0:48:36.810
been no time, energy, or focus for us to come
back and support each other.
0:48:36.810,0:48:44.200
And this, this is a big — what’s the word?
0:48:44.200,0:48:53.650
Like, this fracture is really detrimental
to novice nurses, to newcomers to the profession.
0:48:53.650,0:48:55.990
It’s a really vulnerable time.
0:48:55.990,0:49:02.849
And if they don’t have this, I don’t know
how they’ll stay.
0:49:02.849,0:49:05.150
And the healthcare system depends on them.
0:49:05.150,0:49:09.630
So I really appreciate the urgency that you
researchers are putting into looking at this.
0:49:09.630,0:49:11.780
It’s really, really, really wonderful.
0:49:11.780,0:49:16.290
Thank you.
0:49:16.290,0:49:17.690
Thank you, Michele.
0:49:17.690,0:49:22.849
I want to say that I can feel the emotion
and I was doing a lot of deep breathing as
0:49:22.849,0:49:28.840
you were speaking, and I invite everyone listening
who’s experiencing your story right now to
0:49:28.840,0:49:34.580
take a deep breath — or many, if you need
— and Michele, what I hear from what you’re
0:49:34.580,0:49:39.720
saying is echoes of the fear that Krissha
was talking about, the fear in the workplace,
0:49:39.720,0:49:46.190
and then on top of that, the isolation, which
is so debilitating for people who work as
0:49:46.190,0:49:50.650
a team, and who need to work as a team.
0:49:50.650,0:49:53.560
I would like to turn to Jennifer now.
0:49:53.560,0:50:00.500
You work as a family doctor, and I mentioned
off the top that you also provided COVID charts
0:50:00.500,0:50:04.900
every day on Twitter, which was very useful
for people who were fearful and who wanted
0:50:04.900,0:50:08.690
more information or to know how to understand
the information.
0:50:08.690,0:50:15.250
I know you did that Twitter work above and
beyond your regular job and healthcare professionals
0:50:15.250,0:50:22.089
have been going above and beyond on an individual
level, well, since before the pandemic, but
0:50:22.089,0:50:25.750
also have been asked to do that during this
time.
0:50:25.750,0:50:31.500
What has that been like in your experience
— that constant kind of above and beyond
0:50:31.500,0:50:32.570
feeling?
0:50:32.570,0:50:41.609
Well, thanks to Michele and Krissha for articulating
it so well, that feeling, especially early
0:50:41.609,0:50:45.190
in the pandemic, when there was no vaccines,
right?
0:50:45.190,0:50:48.530
We didn’t even have masks at times.
0:50:48.530,0:50:51.980
I remember even in my clinic, we were like
trying to order more masks.
0:50:51.980,0:50:56.090
We were running low, like how can we protect
our staff and continue to see patients, but
0:50:56.090,0:51:03.240
our supplier — our expect-delivery day,
it kept going back by months.
0:51:03.240,0:51:08.839
So it was that kind of fear that we all felt
initially and I think everyone tried to pitch
0:51:08.839,0:51:13.900
in in whatever way we can, like going beyond
what our regular clinical duties were.
0:51:13.900,0:51:16.900
For myself, I thought, oh, like I can share
information.
0:51:16.900,0:51:20.760
Yeah, it’s not part of my job, but I felt
like that was another way we can all work
0:51:20.760,0:51:21.760
together.
0:51:21.760,0:51:23.839
And I think early pandemic, we all did that.
0:51:23.839,0:51:30.230
Like we all thought about what we can contribute
and have a collective effort to protect our
0:51:30.230,0:51:32.650
patients, protect our families.
0:51:32.650,0:51:37.890
So I think that feeling we all definitely
shared.
0:51:37.890,0:51:43.809
And even now I think the struggle is that
we’re still constantly adapting to the changing
0:51:43.809,0:51:45.000
environment now.
0:51:45.000,0:51:49.210
Like COVID is increasing again, now we have
other respiratory viruses like RSV.
0:51:49.210,0:51:51.320
There’s just so much going on.
0:51:51.320,0:51:53.460
The children’s hospitals are struggling.
0:51:53.460,0:51:59.770
We’re still trying to keep PPE supplies up
and trying to protect our patients.
0:51:59.770,0:52:06.319
For example, we’re still doing outdoor visits
in the parking lot for people who have respiratory
0:52:06.319,0:52:10.240
symptoms, but the weather’s changing, so we
have to adapt to that.
0:52:10.240,0:52:16.030
And it can be difficult because when patients
are sick and struggling, sometimes they’re
0:52:16.030,0:52:23.200
also very upset, and that can affect us and
the staff if people are upset at us.
0:52:23.200,0:52:26.510
But really we shouldn’t be upset at one another.
0:52:26.510,0:52:32.359
We should still continue to try and have that
kind of collective sense of tackling the pandemic
0:52:32.359,0:52:34.109
together.
0:52:34.109,0:52:38.670
Because really I think that’s what everyone’s
grieving, we’re missing our pre-COVID times
0:52:38.670,0:52:44.480
where we didn’t have to have this looming
cloud, like Krissha said, over our heads,
0:52:44.480,0:52:46.920
and just live our lives and be normal.
0:52:46.920,0:52:52.980
But now that we know, it’s been so long, we
just never know when or if that will happen.
0:52:52.980,0:52:59.200
We have to continue to work together and adapt
and support one another through this.
0:52:59.200,0:53:03.920
Thank you, Jennifer.
0:53:03.920,0:53:10.420
You mentioned many things, but one of the
things you mentioned is that people are upset.
0:53:10.420,0:53:15.300
And I saw some data the other day, I don’t
know how they’re measuring it, but there’s
0:53:15.300,0:53:24.030
more rudeness — and I think that probably,
especially as people who deal with the public,
0:53:24.030,0:53:28.000
you probably don’t need a study or research
to show you that.
0:53:28.000,0:53:33.260
I’m just wondering if any one of you would
like to, to tell us about what it’s like to
0:53:33.260,0:53:40.410
be the helper, as we’ve talked about, and
all your energy goes into helping on the job
0:53:40.410,0:53:48.490
— and yet it is such an exhausting job for
all the reasons that you have outlined, needing
0:53:48.490,0:53:57.089
to go above and beyond, needing to really
have part of your mind go to PPE and thinking
0:53:57.089,0:54:07.510
about that, or the lack thereof, thinking
about handling patients who are upset.
0:54:07.510,0:54:09.930
And there are different types of exhaustion
too.
0:54:09.930,0:54:13.470
There’s physical exhaustion, but then there’s
mental exhaustion.
0:54:13.470,0:54:19.330
And I’m wondering if anybody would like to
jump in and just talk about how they handle
0:54:19.330,0:54:25.210
that.
0:54:25.210,0:54:30.000
I can probably provide an example.
0:54:30.000,0:54:42.819
I — there’s not really a way to handle this
huge stressor, I think.
0:54:42.819,0:54:49.589
How I managed to work through it and because
— like when I was in an outbreak situation,
0:54:49.589,0:54:50.920
I was pretty isolated.
0:54:50.920,0:54:53.040
I was away from my family members.
0:54:53.040,0:54:55.359
I had to live in the hotel.
0:54:55.359,0:54:57.980
There was — you’re by yourself.
0:54:57.980,0:55:01.520
You essentially get up to go to work.
0:55:01.520,0:55:06.510
You prepare yourself and you’re — I think
somebody wrote in the comments that they used
0:55:06.510,0:55:10.059
to cry in the car going in.
0:55:10.059,0:55:11.819
That used to be me.
0:55:11.819,0:55:14.910
That used to be how I managed to deal with
it.
0:55:14.910,0:55:21.630
And then, you’re worried about your other
colleagues who were also sick.
0:55:21.630,0:55:29.620
But the only thing you have to do is , you
have to get stuff done.
0:55:29.620,0:55:33.610
Someone has to take care of these people,
because who else is going to take care of
0:55:33.610,0:55:35.830
them, you know?
0:55:35.830,0:55:39.580
We have this like moral thing where we don’t
leave anyone behind.
0:55:39.580,0:55:46.260
We are in this position of power and these
people are so helpless and you treat them
0:55:46.260,0:55:50.420
like family, they’re part of your family.
0:55:50.420,0:55:54.090
You don’t leave anybody behind, so what do
you have to do?
0:55:54.090,0:55:58.289
You have to get up and then you have to do
it.
0:55:58.289,0:56:05.400
You have to put yourself in bootstraps, and
then you have to make a strong face for everyone
0:56:05.400,0:56:11.559
else because the next person you’re looking
at, who you might — they’re also just feeling
0:56:11.559,0:56:13.010
the same way as you are.
0:56:13.010,0:56:18.160
They’re also just breaking down inside, but
they don’t want to show it because they’re
0:56:18.160,0:56:24.180
scared that they’re going to be either stigmatized
or be labeled or whatnot.
0:56:24.180,0:56:28.170
But they’re also kind of like, I don’t want
to break down at work, I’m not that type of
0:56:28.170,0:56:29.170
person.
0:56:29.170,0:56:32.490
They have a lot of pride in their jobs and
they’re really dedicated.
0:56:32.490,0:56:42.160
So yeah, I remember crying because I couldn’t
care for somebody because I had spent so much
0:56:42.160,0:56:43.780
time on another patient.
0:56:43.780,0:56:54.349
And it’s true what they have, the research
shows, it’s, you’re never supposed to be in
0:56:54.349,0:56:59.349
a position where you have to be God.
0:56:59.349,0:57:00.660
You shouldn’t be.
0:57:00.660,0:57:04.859
You shouldn’t have to choose this person lives
and this person dies because you’re only one
0:57:04.859,0:57:10.242
nurse for 32 patients and everyone’s COVID
positive, and you only have a handful of staff,
0:57:10.242,0:57:14.280
and most of the staff are scared for their
own loved ones.
0:57:14.280,0:57:21.990
So I remember me and just the other, the PSW
who showed up for her patients, who’ve known
0:57:21.990,0:57:24.190
them for years and years and years.
0:57:24.190,0:57:28.430
And then we cry in the back and we say, you
know what?
0:57:28.430,0:57:32.160
We have to do, like, we have to take care
of these people.
0:57:32.160,0:57:33.640
Let’s get stuff done.
0:57:33.640,0:57:39.480
Let’s get, if we have to, if we miss some
stuff, what can we do?
0:57:39.480,0:57:40.480
Right?
0:57:40.480,0:57:46.319
Let’s just like, let’s just try our best,
because we are the only one who can help them.
0:57:46.319,0:57:49.299
And then there’s — they can’t even help
themselves.
0:57:49.299,0:57:55.220
And you have family members calling phones
and whatnot and you can’t even use the phone
0:57:55.220,0:57:56.940
because they’re all full of messages.
0:57:56.940,0:58:01.819
And as soon as the one phone rings, it’s like,
“Hi, did you hear about my family member?
0:58:01.819,0:58:02.819
Did you hear?
0:58:02.819,0:58:06.740
I’ve been calling everywhere” and I’m
like, “I’m so sorry.” This is a,
0:58:06.740,0:58:08.450
you can’t provide updates.
0:58:08.450,0:58:09.589
Yeah.
0:58:09.589,0:58:14.720
It’s … what you have to do.
0:58:14.720,0:58:16.480
Every day is like a war.
0:58:16.480,0:58:20.069
You have to put on your — you have to put
on your gear, you have to put on your mask,
0:58:20.069,0:58:21.820
you have to put on your face shield.
0:58:21.820,0:58:27.210
You have to be prepared, like wearing PPE
all the time.
0:58:27.210,0:58:33.340
You’re going to have your … nose marks,
and then you’re going to get severe headache
0:58:33.340,0:58:39.660
because of all the, Hasbro has provided you
with rubber band and a plastic shield and
0:58:39.660,0:58:46.590
stuff, and you’re like, am I — is this COVID,
is this just a headache, or is this just the
0:58:46.590,0:58:47.590
face shield?
0:58:47.590,0:58:49.280
You know?
0:58:49.280,0:58:57.710
And yeah, you have to … sometimes what made
me feel better, was that looking back at patients
0:58:57.710,0:59:01.810
when they were like, at their best, when they
were like laughing, they were just joking
0:59:01.810,0:59:07.810
around or they did some silly thing, or their
family members came and visited and how they
0:59:07.810,0:59:09.380
were reacting.
0:59:09.380,0:59:11.299
Yeah, , and it’s true what Michele said.
0:59:11.299,0:59:13.289
It’s really about camaraderie, right?
0:59:13.289,0:59:23.890
And then this pandemic kind of made us feel
more isolated and really fend for our own.
0:59:23.890,0:59:25.450
And it’s true.
0:59:25.450,0:59:27.250
Like, you go in utility closets.
0:59:27.250,0:59:32.380
I went to the chapel, I cried, and then I
was praying.
0:59:32.380,0:59:34.920
I was like, I hope I don’t get it.
0:59:34.920,0:59:41.130
And I, I hope no one else, you know — sorry,
I have monopolized the time.
0:59:41.130,0:59:44.420
If anyone wants to go, go.
0:59:44.420,0:59:46.869
Never say sorry.
0:59:46.869,0:59:50.000
Your stories are so important to us.
0:59:50.000,0:59:51.770
And Michele, I saw you nodding a lot.
0:59:51.770,0:59:53.250
Is there anything you wanted to add?
0:59:53.250,0:59:55.180
Yeah, and thanks Krissha.
0:59:55.180,0:59:56.849
You’ve really, you captured it.
0:59:56.849,0:59:58.500
It’s for sure what we deal with.
0:59:58.500,1:00:04.740
It’s this, it’s this— I would like to just
put it into a bit of context, because of my
1:00:04.740,1:00:08.770
elder status in the profession.
1:00:08.770,1:00:17.319
I remember when it was a really honourable,
not frantic, human, I might even call it a
1:00:17.319,1:00:18.319
gentle profession.
1:00:18.319,1:00:24.059
You know, in 1990 when I graduated, we had
only begun the defunding.
1:00:24.059,1:00:27.410
Defunding is said to have begun somewhere
in ’85, ’87.
1:00:27.410,1:00:35.840
Our healthcare system has been defunded for
32 years that I’ve been there.
1:00:35.840,1:00:45.920
The impact of consistent, progressive defunding
has come at the expense of — and I’m a bit
1:00:45.920,1:00:52.599
biased and I’m sorry — but nurses, we are
the bulk, physical workers of our healthcare
1:00:52.599,1:00:53.599
system.
1:00:53.599,1:00:55.210
We are the backbone of every hospital.
1:00:55.210,1:00:57.960
If you need a doctor, you go to a doctor’s
office.
1:00:57.960,1:01:00.870
If you’re in a hospital, it’s because you
need a nurse.
1:01:00.870,1:01:01.870
And we have defunded.
1:01:01.870,1:01:08.640
We as a province have chosen to defund healthcare
for 32 years, and it has brought all of us
1:01:08.640,1:01:09.700
to the brink.
1:01:09.700,1:01:17.440
The system now depends on each nurse working
full out and to an exhausted state that I
1:01:17.440,1:01:22.119
have never seen before.
1:01:22.119,1:01:32.150
And it is a malignancy that I think jeopardizes
the future of our healthcare system so fundamentally,
1:01:32.150,1:01:37.650
because nurses are fleeing, because they have
reached their limits.
1:01:37.650,1:01:40.869
They are, we are, all deeply exhausted.
1:01:40.869,1:01:44.080
And what happens with deep exhaustion, is
mistakes happen.
1:01:44.080,1:01:50.360
The moral injuries that do happen in distress
because we’ve made mistakes are real.
1:01:50.360,1:01:52.720
We don’t sleep very well at night.
1:01:52.720,1:01:57.720
We arrive — when, when someone hears a nurse
works 12 hours, it’s a lie.
1:01:57.720,1:02:01.390
I’m at work for 13 hours.
1:02:01.390,1:02:05.490
Our government has betrayed us by Bill 124.
1:02:05.490,1:02:13.099
And our unions haven’t been able to mobilize
any action to be of benefit to us.
1:02:13.099,1:02:19.270
And I just feel like a real threat is looming
at how our hospitals are going to function
1:02:19.270,1:02:27.390
and our healthcare and our nursing homes when
nurses begin to fall because it’s too much.
1:02:27.390,1:02:29.640
We can’t, we’re done.
1:02:29.640,1:02:35.760
We’re, we’re, we’re, we’re, we’re, we’re,
we’re breaking, you know.
1:02:35.760,1:02:41.799
It’s just, it’s, it’s a great urgent grief
and fear of mine.
1:02:41.799,1:02:50.539
I hear so much Michele in what you’re saying
that matches with the research that we have
1:02:50.539,1:02:54.190
been hearing about.
1:02:54.190,1:02:58.960
I hear the sense of betrayal organizationally
speaking.
1:02:58.960,1:03:07.890
I’m wondering if there’s anything else that
anyone on this panel has heard about in terms
1:03:07.890,1:03:11.700
of the definitions of moral injury and moral
distress and the research findings.
1:03:11.700,1:03:18.539
Was there anything else that really struck
you as fitting with your day to day experiences
1:03:18.539,1:03:24.520
at work?
1:03:24.520,1:03:30.819
I guess, one thing I wanted to mention is,
at the end of the day with this defunding
1:03:30.819,1:03:36.619
of the healthcare system, impacting all healthcare
workers, and at the end of the day, it’s the
1:03:36.619,1:03:38.849
patients that are going to suffer, right?
1:03:38.849,1:03:44.410
And sometimes we don’t see it with, it’s not
as immediate, like when you watch someone
1:03:44.410,1:03:48.390
get COVID and get really sick which is very
devastating.
1:03:48.390,1:03:55.619
But sometimes there’s these kind of long,
slow-burning kind of fires.
1:03:55.619,1:04:01.290
So for example, I have patients that would
get like a breast lump and then they have
1:04:01.290,1:04:06.319
to wait for imaging and they have to wait
for biopsy and they have to wait for results.
1:04:06.319,1:04:10.750
And then they have to wait for the specialist
to see them to find out what are the needs,
1:04:10.750,1:04:11.750
surgery or chemo.
1:04:11.750,1:04:16.340
And it’s, it’s so traumatizing to the patient
to have all these weights because the healthcare
1:04:16.340,1:04:18.220
system is so overwhelmed.
1:04:18.220,1:04:23.040
And these are kind of stories that you may
not hear as much because it’s kind of a more
1:04:23.040,1:04:28.089
slow, chronic problem that keeps getting worse.
1:04:28.089,1:04:32.640
For example, pap smears, now it takes like
four months for a result.
1:04:32.640,1:04:35.700
And that’s, what if we’re missing something?
1:04:35.700,1:04:38.010
What if there is something abnormal that needs
to be followed up on?
1:04:38.010,1:04:41.099
And we’re just not even getting results in
time.
1:04:41.099,1:04:47.049
So it, it’s hard because these things are
not as visible, but patient care is impacted
1:04:47.049,1:04:51.170
and when things are delayed, the diagnosis
is delayed.
1:04:51.170,1:04:55.620
Treatment may be more invasive and aggressive
because the cancer is worse.
1:04:55.620,1:05:03.859
So I think that hopefully maybe, if we can
continue to advocate for our professions and
1:05:03.859,1:05:08.030
for proper funding of the healthcare system,
we can avoid a collapse.
1:05:08.030,1:05:12.670
But it’s not looking great in terms of the
trajectory right now.
1:05:12.670,1:05:18.010
And it’s just very sad to see how a lot of
the weight is placed on our shoulders when
1:05:18.010,1:05:23.369
we really need the government to step in and
make things right.
1:05:23.369,1:05:32.460
I’d like to jump in if I can now with a question
from somebody who is here listening.
1:05:32.460,1:05:36.800
Her name is Tracy and she says she manages
a 31-bed unit.
1:05:36.800,1:05:39.770
“I am at 48% staffing.
1:05:39.770,1:05:45.569
My staff are at the breaking point.”
So this is what Michele is describing, and
1:05:45.569,1:05:52.099
Tracy says, “I am seeing toxic interactions
between our core staff and new I.E.N.”
1:05:52.099,1:05:53.900
If someone wants to explain what I.E.N.
1:05:53.900,1:05:58.970
means, I’m sorry, I don’t know, but Tracy
is saying she needs help.
1:05:58.970,1:06:01.109
“I’ve been a nurse for 30 years.
1:06:01.109,1:06:03.380
Is there anything I can do to help all my
staff?”
1:06:03.380,1:06:08.840
This is a very big question, but if there’s
anyone who, Krissha or Michelle or Jennifer,
1:06:08.840,1:06:18.150
if you have a piece of advice for Tracy, she
would like some advice.
1:06:18.150,1:06:20.210
I wish I had advice.
1:06:20.210,1:06:24.180
I wish I knew the answer.
1:06:24.180,1:06:33.460
It’s that your staffing levels are not rare
to have to run with 50% of your full-time
1:06:33.460,1:06:38.609
lines vacant, and no one to work those, that’s
normative now in healthcare.
1:06:38.609,1:06:43.790
What that means, if you don’t know what that
means, it means you work short.
1:06:43.790,1:06:47.940
And if you work 10% short, arguably each nurse
does 10% more work.
1:06:47.940,1:06:51.400
If you’re 20% short, you’re doing 20% more.
1:06:51.400,1:06:52.400
30% short.
1:06:52.400,1:06:54.720
So her unit’s running at 50% short.
1:06:54.720,1:06:56.650
That’s not surprising to me.
1:06:56.650,1:06:59.819
That’s probably where most of our emerg systems
are at.
1:06:59.819,1:07:04.349
And at that rate, the nurses who are coming
on, are working 50% more — because there’s
1:07:04.349,1:07:05.510
not fewer people.
1:07:05.510,1:07:09.270
Our population has grown while our funding
has shrunk.
1:07:09.270,1:07:16.750
So I think being a manager who cares and can
hear and can do their very best to support
1:07:16.750,1:07:23.069
and can recognize how everybody who does show
up tries their best and works their hardest.
1:07:23.069,1:07:27.950
I really appreciate when my boss says to me,
Michele, thank you for coming to work.
1:07:27.950,1:07:29.150
Thank you for showing up.
1:07:29.150,1:07:31.180
Thank you so much for staying late.
1:07:31.180,1:07:34.950
Thank you for everything you do.
1:07:34.950,1:07:38.529
It is pretty, pretty important to be thanked.
1:07:38.529,1:07:43.710
So that’s like the smallest thing I can suggest.
1:07:43.710,1:07:46.650
And I think Tracy, you’re not alone.
1:07:46.650,1:07:53.109
There’s every manager, every nursing unit
manager is dealing with this identical problem,
1:07:53.109,1:08:01.270
and the ability to affect an improvement is
really, really going to be difficult …
1:08:01.270,1:08:06.309
What I see is the fracture when she speaks
of senior nurses [who are] aggressive at each
1:08:06.309,1:08:07.309
other.
1:08:07.309,1:08:08.799
There’s a real fracture of relationships.
1:08:08.799,1:08:14.089
And this kind of, what I described as this
kind of thing, we used to stick together and
1:08:14.089,1:08:16.210
now — I have done it.
1:08:16.210,1:08:20.029
I have snapped at my fellow senior nurses.
1:08:20.029,1:08:27.359
I’ve snapped, and I’ve been — we now isolate
just so that we can self-regulate.
1:08:27.359,1:08:33.120
And we used to co-regulate and now we self-regulate
and it’s — we’ve lost an ability.
1:08:33.120,1:08:39.330
We’ve lost our way to find that relationship
when that’s fundamental to how we get through
1:08:39.330,1:08:40.330
our days.
1:08:40.330,1:08:45.790
And without that, we can hire new nurses,
but they don’t stay because there’s not a
1:08:45.790,1:08:47.390
network of support for them.
1:08:47.390,1:08:50.520
They are even more isolated and more afraid.
1:08:50.520,1:08:54.080
And it’s like a problem that’s like a snowball
going down a hill.
1:08:54.080,1:08:58.660
It’s getting bigger and bigger because as
people leave, there’s more work, as there’s
1:08:58.660,1:09:04.260
more work, there’s less support, there’s less
support, there’s less processing of the injury.
1:09:04.260,1:09:05.589
That’s part of our job.
1:09:05.589,1:09:07.549
Moral distress is part of our job.
1:09:07.549,1:09:12.230
It’s part of the, it’s part of the water we
swim in.
1:09:12.230,1:09:21.710
Like, there’s just no way you can be a nurse
and not have experienced this.
1:09:21.710,1:09:29.960
It’s just COVID tipped the balance in such
a negative way, and I think the people who
1:09:29.960,1:09:35.750
are studying nursing and healthcare workers’
traumas prior to COVID, I think the numbers
1:09:35.750,1:09:39.469
are probably there saying, yeah, the traumas
have been there all along.
1:09:39.469,1:09:44.949
But COVID certainly has just tipped it all,
the balance not in our favour.
1:09:44.949,1:09:47.009
So stay strong Tracy.
1:09:47.009,1:09:51.640
And I think love in the nurses you have is
already pretty great because, well, it’s kind
1:09:51.640,1:09:52.900
of all we can do.
1:09:52.900,1:09:53.900
I’m —
1:09:53.900,1:09:56.430
That’s great advice, Michele.
1:09:56.430,1:09:57.430
Thanks.
1:09:57.430,1:09:59.949
Yes, please finish your sentence.
1:09:59.949,1:10:01.280
I didn’t mean to cut you off.
1:10:01.280,1:10:02.300
Oh, it’s okay.
1:10:02.300,1:10:05.490
Nurses, we create nursing care plans for our
patients.
1:10:05.490,1:10:08.730
It’s kind of, if you’re a nurse, you know
what I’m talking about, that it’s what we
1:10:08.730,1:10:11.470
do to sort of, we create a nursing care plan.
1:10:11.470,1:10:16.790
And I have this wish that as nurses we can
create a nursing care plan for nurses that
1:10:16.790,1:10:21.600
we can figure out, cause our job’s so unique
and it’s so misunderstood.
1:10:21.600,1:10:24.010
We’re not represented in media.
1:10:24.010,1:10:25.500
People don’t understand what nurses do.
1:10:25.500,1:10:30.230
I feel like only nurses understand just what
we do, cause we’re there.
1:10:30.230,1:10:31.590
Anybody can follow me around for 12 hours.
1:10:31.590,1:10:32.590
I welcome you.
1:10:32.590,1:10:33.590
Please come.
1:10:33.590,1:10:37.810
I’ll try to help you understand what nurses
do, but I really would love to see us be able
1:10:37.810,1:10:45.860
to find a way to care for ourselves because
our problems are pretty unique in our environment
1:10:45.860,1:10:49.760
and our, our, our challenges are unique.
1:10:49.760,1:10:52.679
So that’s it.
1:10:52.679,1:10:58.780
I really hope that some of the recommendations
that Andrea had shared earlier can be like
1:10:58.780,1:11:03.760
a nurse’s, like a plan that you’re talking
about, a care plan.
1:11:03.760,1:11:09.840
I am running just a couple of minutes late
in our agenda, but I do want to close this
1:11:09.840,1:11:15.239
panel, which honestly, I could keep listening
to you for so long, I know that you have so
1:11:15.239,1:11:19.740
many stories and experiences that are very
illuminating.
1:11:19.740,1:11:25.429
But it, it, it, I don’t want to seem trite,
but I do want to end on some sort of a positive
1:11:25.429,1:11:31.071
note in terms of, when we started our panel,
we talked about what you love about the job,
1:11:31.071,1:11:35.650
and then we talked about the immense hardships
that you face every day.
1:11:35.650,1:11:40.659
And Krissha, you mentioned, you just have
to do it.
1:11:40.659,1:11:42.389
You just have to deliver the patient care.
1:11:42.389,1:11:43.850
You just do it.
1:11:43.850,1:11:46.699
You hug your colleague and you just keep going.
1:11:46.699,1:11:52.350
So I’m wondering, briefly, if everyone can
mention what is the one thing or what is a
1:11:52.350,1:11:59.820
thing that does keep you going, that can recharge
you reliably so you can continue to work.
1:11:59.820,1:12:02.610
And it’s in the spirit of the advice for Tracy.
1:12:02.610,1:12:10.469
You know, I would love to hear from all of
you, one thing that does that for you.
1:12:10.469,1:12:19.010
I see Krissha’s thinking, so I’ll leave her
for a moment.
1:12:19.010,1:12:21.830
Yeah, I’m going to be thinking.
1:12:21.830,1:12:22.830
Yeah.
1:12:22.830,1:12:25.110
It’s like a deep, dark dive.
1:12:25.110,1:12:26.110
Sorry.
1:12:26.110,1:12:27.110
Jennifer, would you like to start?
1:12:27.110,1:12:29.930
Sure, I can start.
1:12:29.930,1:12:35.960
I think one thing that keeps me going is that
when patients are at their most vulnerable,
1:12:35.960,1:12:43.450
when they’re sick and in distress, they need
someone to be there to be that calm, reliable
1:12:43.450,1:12:44.450
person.
1:12:44.450,1:12:49.650
And even though sometimes we don’t feel that
way, we’re struggling too, and we’re working
1:12:49.650,1:12:55.790
with limited resources, but the patient still
needs someone to be there for them that can
1:12:55.790,1:12:57.370
help them navigate the system.
1:12:57.370,1:12:59.330
And at the end of the day, that’s our job.
1:12:59.330,1:13:01.080
We need to help people.
1:13:01.080,1:13:02.080
We want to help people.
1:13:02.080,1:13:06.130
That’s why we came into the profession, whether
as a doctor or nurse or any other healthcare
1:13:06.130,1:13:07.130
provider.
1:13:07.130,1:13:10.310
And that’s what we will continue to do.
1:13:10.310,1:13:15.880
And that keeps me going because no one else
can be that person for that patient in that
1:13:15.880,1:13:23.780
time, and it’s just an honour to be in that
role.
1:13:23.780,1:13:24.780
Thank you.
1:13:24.780,1:13:26.560
And Michele?
1:13:26.560,1:13:33.800
I think when I spoke of what I love about
the profession, it’s still there.
1:13:33.800,1:13:36.320
All of what I spoke of is still there.
1:13:36.320,1:13:43.469
It’s not gone.
1:13:43.469,1:13:47.760
And so I only, it’s fracturing, but it’s not
gone and it’s still there and it’s still what
1:13:47.760,1:13:56.850
brings a lot of joy to all of our hearts,
that ability to be a team that comes together
1:13:56.850,1:13:59.699
and helps someone who’s in distress.
1:13:59.699,1:14:08.469
Who brings our incredible critical thinking
skills, our incredible scientific understanding,
1:14:08.469,1:14:17.639
our hands-on technical skills, when we can
do right by our patients, it’s a very glorious
1:14:17.639,1:14:18.639
moment.
1:14:18.639,1:14:27.500
And I think those still happen for sure, and
they’re still pretty rewarding moments.
1:14:27.500,1:14:34.409
I echo the same as Michele and Jennifer.
1:14:34.409,1:14:46.660
What keeps me going is a lot of coffee and
a lot of self-talk that like, you can do this,
1:14:46.660,1:14:51.870
you were put in this earth for a purpose.
1:14:51.870,1:14:53.250
And it’s true … what Michelle said.
1:14:53.250,1:14:54.270
It is a bit fractured.
1:14:54.270,1:14:59.460
cause now I see it in a different way now.
1:14:59.460,1:15:03.050
However, the only thing I can do is do right.
1:15:03.050,1:15:09.150
Do right by your patients, make your own difference.
1:15:09.150,1:15:11.699
And that’s what keeps me going.
1:15:11.699,1:15:14.239
I’m just like, I’m here to do my job.
1:15:14.239,1:15:21.050
I’m here to take care of this person … during
this shift, and that’s my responsibility.
1:15:21.050,1:15:24.830
And I will take care of them to the best of
my ability.
1:15:24.830,1:15:31.950
And yeah, because I, there’s now for me, I
no longer have trust with the system.
1:15:31.950,1:15:39.699
I now, I’m not very, I don’t trust the system,
I don’t think it works for any of us or for
1:15:39.699,1:15:43.219
the patients and for their own health and
safety.
1:15:43.219,1:15:46.770
So I have a lot of, I’m quite cautious.
1:15:46.770,1:15:53.040
I’m always, it’s terrible now, because I’m,
I’m more like a, kind of like a cynic now
1:15:53.040,1:15:54.090
because I don’t trust it.
1:15:54.090,1:16:00.190
But it doesn’t mean that, it doesn’t always,
it’s not always negative, it’s always positive.
1:16:00.190,1:16:06.300
So what I always think about is my patients
being discharged, walking out of there and
1:16:06.300,1:16:15.830
being, like having done something to promote
their own health, and making a really — and
1:16:15.830,1:16:21.260
also I find that they’ve also spoken to us
and really understand like, you guys are really
1:16:21.260,1:16:23.330
short, you guys are super short-staffed.
1:16:23.330,1:16:28.280
And they understand and they give us, and
they’re, they empathize with us and they say,
1:16:28.280,1:16:29.280
“I’m so sorry.
1:16:29.280,1:16:34.090
I’m not going to try to call, but I just need
this one thing.” And I’m like, “It’s
1:16:34.090,1:16:35.090
okay.
1:16:35.090,1:16:36.090
It’s fine.
1:16:36.090,1:16:41.040
You know, you need something, you need something.”
But they’re really, and I, and I appreciate
1:16:41.040,1:16:42.040
that.
1:16:42.040,1:16:43.040
I really do.
1:16:43.040,1:16:50.850
And I also appreciate them not voting for
Doug Ford, but that’s usually how we do it
1:16:50.850,1:16:52.980
during campaign season.
1:16:52.980,1:16:55.909
But yeah.
1:16:55.909,1:16:58.349
And yeah, sharing a laugh with them.
1:16:58.349,1:17:02.699
I don’t know if you guys notice, I really
like to laugh and that’s one of my thing is
1:17:02.699,1:17:10.760
just making people laugh and making my patients
laugh and I, that’s what keeps me going, is
1:17:10.760,1:17:16.159
at least like during their time of need, I
can always at least try to make them laugh,
1:17:16.159,1:17:23.050
and put a positive spin on a negative situation.
1:17:23.050,1:17:24.930
Your patients are lucky to have you.
1:17:24.930,1:17:29.820
And I say that to you Krissha and to you Michelle,
and to you Jennifer.
1:17:29.820,1:17:33.420
And I want to echo the feelings that are coming
through the chat.
1:17:33.420,1:17:36.060
There are many hearts and many thank yous.
1:17:36.060,1:17:43.650
I wish I could say thank you in an even bigger
way, but just, I hope you can see in the chat
1:17:43.650,1:17:49.389
that people are so appreciative of the space,
of the stories you’ve shared, and that you
1:17:49.389,1:17:54.520
brought your whole selves to this conversation,
which I’m sure was not easy though.
1:17:54.520,1:17:57.900
So thank you very, very much for today.
1:17:57.900,1:18:00.140
Thank you.
1:18:00.140,1:18:06.280
And I would like to tell everybody who is
here, please take this opportunity to have
1:18:06.280,1:18:09.860
a very quick break.
1:18:09.860,1:18:14.150
It’s meant to be five minutes, but maybe we’ll
even shorten it to three minutes.
1:18:14.150,1:18:15.150
We’ll see.
1:18:15.150,1:18:18.550
This is your time to grab a glass of water
if you need.
1:18:18.550,1:18:24.739
Also in the chat, I encourage everyone to
drop one word to just say how you’re feeling
1:18:24.739,1:18:26.010
at the end of that panel.
1:18:26.010,1:18:30.530
It would be really nice to connect or feel
that connection with everybody else who’s
1:18:30.530,1:18:31.530
here.
1:18:31.530,1:18:32.530
How are you feeling?
1:18:32.530,1:18:34.080
How are you doing?
1:18:34.080,1:18:38.909
So we’ll be on a quick break and then we’ll
come back with another panel with healthcare
1:18:38.909,1:18:40.880
researchers on this topic.
1:18:40.880,1:18:43.440
Thank you very much.
1:18:43.440,1:18:44.440
Hello.
1:18:44.440,1:18:49.110
And we’re coming back from the break.
1:18:49.110,1:18:52.989
Thank you so much to everybody who is keeping
the chat going.
1:18:52.989,1:19:00.110
I really enjoyed reading the comments, trying
to stay on top of them, but I’m so happy to
1:19:00.110,1:19:07.520
see how people are sharing what that last
panel felt like, to be a part of that conversation,
1:19:07.520,1:19:09.239
to be hearing the conversation.
1:19:09.239,1:19:15.130
A lot of feeling connected and recognized
and inspired and empowered.
1:19:15.130,1:19:20.699
So thank you everybody who is listening and
participating.
1:19:20.699,1:19:26.590
Now we are going to go to another panel this
time with researchers.
1:19:26.590,1:19:31.659
This panel is on risk and mitigating factors
of moral injury and moral distress and Canadian
1:19:31.659,1:19:34.090
healthcare providers during the pandemic.
1:19:34.090,1:19:41.050
So I’d like to introduce Mahée Gilbert-Ouimet
in Quebec, Michelle McCarron in Saskatchewan,
1:19:41.050,1:19:44.969
and Margaret McKinnon is coming back for this
panel as well.
1:19:44.969,1:19:50.800
So you three will be bringing your research
to this conversation, and I’ll go to each
1:19:50.800,1:19:55.050
one of you one at a time to describe your
research a little, and then we can open it
1:19:55.050,1:19:57.409
up for some conversation.
1:19:57.409,1:20:03.280
But first of all, I just want to know if anybody
has a quick reaction to what you heard in
1:20:03.280,1:20:07.280
the panel before the break.
1:20:07.280,1:20:08.760
I see Margaret nodding.
1:20:08.760,1:20:11.090
Maybe you would like to start.
1:20:11.090,1:20:12.090
Thank you, Hannah.
1:20:12.090,1:20:16.610
And you know, I don’t think we can say strongly
enough to our healthcare workers who spoke
1:20:16.610,1:20:19.170
today thank you for your courage.
1:20:19.170,1:20:25.530
We see reflected in the comments just how
much people are hearing, heard, recognized,
1:20:25.530,1:20:33.520
valued, and I think giving people words to
describe experiences are very powerful.
1:20:33.520,1:20:39.020
So hearing about moral injury, often people
say it helps me to realize I’m not alone,
1:20:39.020,1:20:43.350
that others are experiencing this, and we’re
hearing that in the chat today.
1:20:43.350,1:20:51.070
It also is a reflection of the incredible
service that nurses, physicians, occupational
1:20:51.070,1:20:57.050
therapists, environmental service workers,
admin assistants, everyone in the system has
1:20:57.050,1:20:58.050
given.
1:20:58.050,1:21:02.040
I can tell you that during the pandemic when
people were talking about the utility closets,
1:21:02.040,1:21:03.420
that rang so true.
1:21:03.420,1:21:09.920
I was in a COVID unit for a day and a half,
and I actually sat in the utility closet while
1:21:09.920,1:21:15.190
people changed their masks to provide mental
healthcare because of the only time those
1:21:15.190,1:21:18.690
healthcare workers had to receive care.
1:21:18.690,1:21:25.949
So I just feel that we cannot thank you enough
to all of you in the audience and to our panelists
1:21:25.949,1:21:30.370
for sharing your stories and for your courage
and your sacrifices.
1:21:30.370,1:21:33.230
So thank you.
1:21:33.230,1:21:35.330
Absolutely.
1:21:35.330,1:21:42.260
And Mahée or Michelle, would you like to
provide any reaction to what we just heard.
1:21:42.260,1:21:43.260
Yes.
1:21:43.260,1:21:50.929
Well, like Margaret, I want to thank you for
speaking up, for being there with us today.
1:21:50.929,1:21:53.440
I am an epidemiologist.
1:21:53.440,1:22:00.320
I work on stress at work among various population,
but the project that I’m going to speak to
1:22:00.320,1:22:06.370
you about in the next minute was my first
experience with moral injury.
1:22:06.370,1:22:13.810
And what I was not planning to say was that
I cried a lot when I was reading after the
1:22:13.810,1:22:16.360
interviews that I performed.
1:22:16.360,1:22:22.890
It was really hard and it’s kind of coming
up when I hear you speak.
1:22:22.890,1:22:25.179
So it’s a very humbling experience.
1:22:25.179,1:22:29.560
I admire you and I want to thank you.
1:22:29.560,1:22:37.870
And I, I just want to really echo what Margaret
and Mahée said about thanking the panelists,
1:22:37.870,1:22:41.480
the healthcare providers, for sharing their
stories.
1:22:41.480,1:22:48.790
It’s really so powerful hearing these stories
from you in your own words and how this experience
1:22:48.790,1:22:50.470
has impacted you.
1:22:50.470,1:22:58.930
And I had the same experience when I did research
in this area, that it brought tears to my
1:22:58.930,1:22:59.930
eyes, honestly.
1:22:59.930,1:23:07.370
Doing the interviews and then reading through
transcripts after, because just the amount
1:23:07.370,1:23:16.060
that people were impacted by their experiences
providing healthcare in those very trying
1:23:16.060,1:23:23.310
times, and the sustained impact it was having
on them, the cumulative impact, was really
1:23:23.310,1:23:24.310
powerful.
1:23:24.310,1:23:29.719
Yet they kept showing up day after day and
still doing this and trying to provide the
1:23:29.719,1:23:32.489
best care possible for patients.
1:23:32.489,1:23:39.710
And I heard those same themes echoed amongst
the healthcare panelists today, that strong
1:23:39.710,1:23:43.969
commitment to caring for patients really,
really comes through.
1:23:43.969,1:23:45.980
So thank you for that.
1:23:45.980,1:23:47.460
Yeah.
1:23:47.460,1:23:54.160
And I would like to add that for the panelists,
I was saying that there’s almost no way to
1:23:54.160,1:24:00.070
verbalize how much gratitude you feel when
you hear the stories communicated.
1:24:00.070,1:24:05.780
So please know that these are the kinds of
things we think about later, as Mahée said,
1:24:05.780,1:24:09.380
part of your research, we, your stories really
stay.
1:24:09.380,1:24:15.620
And I’m sorry, I’m just going to do this now
because we’ve been talking for so long the
1:24:15.620,1:24:19.380
batteries have died, so I, as long as you
can still hear me.
1:24:19.380,1:24:20.380
Yes?
1:24:20.380,1:24:27.230
I want to get right into the research that
all three of you are bringing to the panel.
1:24:27.230,1:24:29.140
Michelle, can we start with you?
1:24:29.140,1:24:34.440
If you want to briefly tell us about your
research and what types of stressors people
1:24:34.440,1:24:37.560
were describing to you in terms of their work
in healthcare?
1:24:37.560,1:24:38.560
Absolutely.
1:24:38.560,1:24:39.560
Thank you, Hannah.
1:24:39.560,1:24:44.989
And just before I get started, I do want to
acknowledge that I’m speaking to you from
1:24:44.989,1:24:47.989
Treaty 4 territory in Regina.
1:24:47.989,1:24:55.119
So my team and I did a qualitative study,
interview study, with healthcare providers
1:24:55.119,1:24:57.950
in the summer of 2021.
1:24:57.950,1:25:04.980
Wanting to learn more about their experiences
of providing healthcare during the pandemic
1:25:04.980,1:25:11.180
and the stressors that they were experiencing,
the workplace and the moral distress and experiences
1:25:11.180,1:25:13.590
of moral injury that arose from those.
1:25:13.590,1:25:21.380
So we conducted this study with 37 frontline
healthcare workers, whom we interviewed across
1:25:21.380,1:25:22.380
Saskatchewan.
1:25:22.380,1:25:27.710
It was supported by an IDEaS grant from the
Department of National Defence, and we had
1:25:27.710,1:25:32.250
the opportunity to speak with people in a
variety of roles.
1:25:32.250,1:25:37.441
So nurses, doctors, people in various types
of therapist positions, hospital food service
1:25:37.441,1:25:44.179
workers — so really trying to get a broad
spectrum of frontline healthcare providers.
1:25:44.179,1:25:46.610
And we also spoke to people from across the
province.
1:25:46.610,1:25:53.210
So we had a really good mix of rural, northern,
and urban healthcare providers and in a variety
1:25:53.210,1:25:54.790
of healthcare settings.
1:25:54.790,1:25:59.989
So in hospital, long-term care, or public
health, for example.
1:25:59.989,1:26:05.750
So we had representation from all of these
different parts of the province and people
1:26:05.750,1:26:08.489
and working in all sorts of roles.
1:26:08.489,1:26:14.610
Yet, there were a lot of types of workplace
stressors that people were bringing up to
1:26:14.610,1:26:17.969
us consistently when they were telling their
stories.
1:26:17.969,1:26:25.250
So some of these were preexisting the pandemic
and were exacerbated by the situations in
1:26:25.250,1:26:26.250
the pandemic.
1:26:26.250,1:26:32.790
So things like increased overtime, the regular
communication barriers that can arise when
1:26:32.790,1:26:37.929
you’re working in a large healthcare organization,
and particularly when directives were changing
1:26:37.929,1:26:44.350
so rapidly, particularly in the early days
of COVID, the stressors that come with working
1:26:44.350,1:26:53.510
in a fast-paced very high-charge, high-stakes
environment, and not always agreeing with
1:26:53.510,1:26:59.130
some of the decisions being made by leadership
about the different directives that they had
1:26:59.130,1:27:00.410
to follow.
1:27:00.410,1:27:06.909
So there were workplace stressors like that,
but there were also some workplace stressors
1:27:06.909,1:27:12.969
people described that were really novel for
them arising from the pandemic.
1:27:12.969,1:27:22.199
So things like staff redeployments to ensure
that coverage was in areas of greatest need.
1:27:22.199,1:27:29.370
Things that really they felt was impacting
the quality of the patient care that they
1:27:29.370,1:27:30.460
could provide.
1:27:30.460,1:27:37.480
So reducing or temporarily shutting down entire
services, delaying surgeries.
1:27:37.480,1:27:43.110
So if they weren’t emergent, then they were
typically delayed in a lot of cases.
1:27:43.110,1:27:48.520
And people said that these might not be seen
on paper as urgent, but they still really
1:27:48.520,1:27:50.900
impact the quality of life of patients.
1:27:50.900,1:27:56.400
And having to hear how much they were suffering
because of these delays was really taking
1:27:56.400,1:27:57.560
a toll on them.
1:27:57.560,1:28:03.900
And then there were things like enforcing
visitor restrictions, and this is one that
1:28:03.900,1:28:05.631
came up over and over again.
1:28:05.631,1:28:11.300
And particularly, I was hearing lots of stories
from people who were working in long-term
1:28:11.300,1:28:18.889
care settings and they kept bringing up the
experiences of working there at Christmas
1:28:18.889,1:28:19.960
time in 2020.
1:28:19.960,1:28:23.719
So these interviews were conducted in the
summer of 2020.
1:28:23.719,1:28:31.870
And it was really heartbreaking for people
to have to keep residents from visiting with
1:28:31.870,1:28:33.830
their family members.
1:28:33.830,1:28:42.780
So they understood the logic behind the rules
that need to try to prevent the spread of
1:28:42.780,1:28:43.780
COVID.
1:28:43.780,1:28:50.800
But people kept telling me that there’s that
physically protecting residents, but then
1:28:50.800,1:28:56.030
what about the psychosocial impacts, and the
impacts to their overall quality of life and
1:28:56.030,1:28:57.429
to their families?
1:28:57.429,1:29:03.230
And sometimes people wondered if the trade
off was worth it because they saw people suffering
1:29:03.230,1:29:04.670
in other ways so much.
1:29:04.670,1:29:12.570
So sometimes people would find some creative
workarounds for the rules and try to enforce
1:29:12.570,1:29:16.389
the spirit of the law, if not the letter of
the law, per se.
1:29:16.389,1:29:22.369
So there’s a story one time of someone that
said that they, they didn’t care if they were
1:29:22.369,1:29:25.880
going to get in trouble for this, but they
weren’t going to keep this family from seeing
1:29:25.880,1:29:26.880
the patient.
1:29:26.880,1:29:31.159
So they had the family stand in the doorway
and the foyer.
1:29:31.159,1:29:33.370
So there was still the inner doors there.
1:29:33.370,1:29:39.770
They still had the resident physically distanced,
but they were at least able to speak to each
1:29:39.770,1:29:41.750
other and see each other.
1:29:41.750,1:29:46.600
If people dropped off packages at that time,
they were supposed to hold them for 24 hours
1:29:46.600,1:29:48.159
before delivering them.
1:29:48.159,1:29:55.119
Just in case — because again, not sure how
much could be transmitted from passing packages
1:29:55.119,1:29:56.170
along.
1:29:56.170,1:30:00.540
So there was one person who said that, when
families dropped off packages on Christmas
1:30:00.540,1:30:05.060
Day, they weren’t going to withhold those
from residents on Christmas.
1:30:05.060,1:30:12.909
So they took sanitary wipes, wiped the packages
down thoroughly, and delivered them.
1:30:12.909,1:30:16.580
So trying to find those compromises.
1:30:16.580,1:30:24.350
There were these stories, these examples of
people who were experiencing these moral dilemmas
1:30:24.350,1:30:31.530
about do I do what I feel is really right
for my patients and residents versus do I
1:30:31.530,1:30:34.280
follow the directives to the letter?
1:30:34.280,1:30:40.310
And people were really struggling with what
that brought up for them and wrestling with
1:30:40.310,1:30:42.420
those types of decisions.
1:30:42.420,1:30:46.730
So that, that was a really big overarching
theme there.
1:30:46.730,1:30:51.860
So maybe I’ll just stop it there for now so
I can let other people have a chance to speak,
1:30:51.860,1:30:55.949
but I’m sure we’ll come back to this at some
point.
1:30:55.949,1:30:56.949
Yes.
1:30:56.949,1:30:57.949
Thank you Michelle.
1:30:57.949,1:31:04.639
And I would like to go to Mahée because you
also did research on moral injury based on
1:31:04.639,1:31:07.739
interviews with healthcare workers in Quebec.
1:31:07.739,1:31:13.989
Were you hearing a lot of the same types of
stories, or can you tell us about the stressors
1:31:13.989,1:31:17.460
that healthcare workers were describing to
you?
1:31:17.460,1:31:18.460
Absolutely.
1:31:18.460,1:31:19.490
Thank you Hannah.
1:31:19.490,1:31:20.950
And thank you Michelle.
1:31:20.950,1:31:27.500
Yes, there are definitely overlaps between
what we shared, what we observed in our research,
1:31:27.500,1:31:34.430
so a little context for you to understand
what my team and I did.
1:31:34.430,1:31:43.450
So we led a research project among 572 frontline
healthcare workers during the third wave of
1:31:43.450,1:31:46.489
the pandemic, so also during the summer of
2021.
1:31:46.489,1:31:51.190
The project was also funded by the Ministry
of Defence of Canada.
1:31:51.190,1:31:55.230
Participants, there were two phases of the
study.
1:31:55.230,1:32:02.150
So participants first completed a quantitative
questionnaire, mainly focusing on psychosocial
1:32:02.150,1:32:10.040
stressors at work and mental health problems,
including moral injury and a subgroup of them
1:32:10.040,1:32:18.150
then were invited to be involved in qualitative
interviews to get a deeper understanding of
1:32:18.150,1:32:23.420
the events and emotions that led to moral
injuries.
1:32:23.420,1:32:31.250
So in the quantitative component of the study,
the stressor that I really want to speak about
1:32:31.250,1:32:38.650
today is the stressor that had the highest
adverse association with moral injury.
1:32:38.650,1:32:43.590
It was the lack of ethical culture in the
workplace.
1:32:43.590,1:32:51.330
It’s not surprising in our sample participants
working in a setting lacking ethical culture
1:32:51.330,1:33:00.040
had five times more risk of moral injury compared
to workers benefiting from a strong or adequate
1:33:00.040,1:33:02.300
ethical culture at work.
1:33:02.300,1:33:06.620
So you might wonder what are we calling a
lack of ethical culture?
1:33:06.620,1:33:14.130
So we asked a series of questions like, in
general, unethical situations that arise at
1:33:14.130,1:33:19.860
work or not discussed transparently with those
directly involved.
1:33:19.860,1:33:26.710
We also asked in general, analytical situation
that arise at work are not constructively
1:33:26.710,1:33:31.500
presented and openly discussed with the rest
of the workplace.
1:33:31.500,1:33:38.219
So we spoke about debriefing, the importance
of the debriefing with the team.
1:33:38.219,1:33:46.800
So in qualitative interviews, to give you
an example of a verbatim a participant reported,
1:33:46.800,1:33:53.929
“If I think about the profession that
I’m doing, a value that they told us so much
1:33:53.929,1:34:00.500
about during our university studies was that
if you are doing something, do it right, do
1:34:00.500,1:34:04.100
it neutral, but do not harm.
1:34:04.100,1:34:11.230
By obeying the directives, I consider myself
doing harm.” So it kind of resonates
1:34:11.230,1:34:15.170
with what we heard before the pause.
1:34:15.170,1:34:21.969
So this testimony was aligned with other events
that were reported by participants.
1:34:21.969,1:34:34.040
Events involved being unable to provide appropriate
care, even basic one, because of lack of resources.
1:34:34.040,1:34:40.440
We were also told about the inability to apply
security measures and directives related to
1:34:40.440,1:34:48.940
COVID-19, being unable to ensure your own
security, but also patients’ safety and not
1:34:48.940,1:34:52.070
being adequately supervised.
1:34:52.070,1:34:59.400
And this was reported a lot when speaking
about movements from units to units and having
1:34:59.400,1:35:05.670
to sometimes switch specialty and not being
adequately trained.
1:35:05.670,1:35:15.150
So these events were linked to a moral injury
through emotions like frustration, anger,
1:35:15.150,1:35:24.560
guilt, shame, helplessness, feelings of worthlessness,
isolation, or deconsolidation of the work,
1:35:24.560,1:35:33.219
collective feeling of injustice and betrayal,
like Margaret spoke about feeling of incompetence,
1:35:33.219,1:35:38.010
sadness, and also sometimes loss of meaning.
1:35:38.010,1:35:44.650
So I’m going to finish my short intervention
about the values that were reported as hurt.
1:35:44.650,1:35:55.160
They reported that professionalism was hurt,
patient and self safety, compassion, kindness,
1:35:55.160,1:35:56.630
and humanity.
1:35:56.630,1:36:06.340
So I’m finishing this little testimony by
reiterating the importance of ethical culture,
1:36:06.340,1:36:11.200
at least in our research project.
1:36:11.200,1:36:17.200
Thank you so much for that Mahée and for
describing what an ethical culture looks like,
1:36:17.200,1:36:22.840
which it, it sounds like a lot of communication
and understanding— like recognizing the
1:36:22.840,1:36:26.139
humanity of the people who do the jobs that
we need done.
1:36:26.139,1:36:30.130
Margaret, I would like to turn to you now.
1:36:30.130,1:36:35.440
Earlier when you were speaking with us, we
talked about moral injury, what it meant,
1:36:35.440,1:36:37.010
what an injury meant.
1:36:37.010,1:36:42.570
I would like to talk about the, or have you
talk about the neuroscience around trauma.
1:36:42.570,1:36:47.580
Can you describe what effect moral injury
has on our brains?
1:36:47.580,1:36:48.580
Yeah, I certainly can.
1:36:48.580,1:36:54.010
And Hannah, if you don’t mind, I’m just going
to follow up a little bit of what we said
1:36:54.010,1:36:57.210
already and then turn to that question if
that’s alright.
1:36:57.210,1:37:01.639
I think what we’ve heard from Mahée and Michelle
is very much what we also heard across the
1:37:01.639,1:37:02.639
country.
1:37:02.639,1:37:07.500
We conducted 134 qualitative interviews and
heard very similar themes, which I think speaks
1:37:07.500,1:37:12.199
to … those experiences that buying Canadian
healthcare workers together.
1:37:12.199,1:37:17.590
And we know that one of the most protective
factors against the development of post-traumatic
1:37:17.590,1:37:21.420
stress disorder in the face of situations
like this is social support.
1:37:21.420,1:37:28.619
So being able to speak to one another, to
hear one another’s stories, to provide empathy
1:37:28.619,1:37:29.990
and caring and support.
1:37:29.990,1:37:35.190
And so I think part of what our job is in
the Canadian healthcare system right now,
1:37:35.190,1:37:41.110
is to recognize the organizational and systemic
factors that are impacted upon healthcare
1:37:41.110,1:37:44.909
workers and to provide the supports to bring
the system back together again to bring the
1:37:44.909,1:37:47.130
family back together again, essentially.
1:37:47.130,1:37:51.449
We’ve done similar interviews in public safety
personnel, which we’ll be holding another
1:37:51.449,1:37:53.780
symposium on later in the year to talk about.
1:37:53.780,1:37:59.719
But I also want to say that when we looked
at what are the factors that are driving departures
1:37:59.719,1:38:04.830
from the healthcare workforce right now, and
we heard a lot about that from Michele, from
1:38:04.830,1:38:11.280
Krissha, and also from Jennifer, we found
that moral distress is what’s driving the
1:38:11.280,1:38:15.199
decision of one in two healthcare workers
who are currently considering leaving their
1:38:15.199,1:38:16.250
clinical positions in Canada.
1:38:16.250,1:38:21.340
And so when we look at the number one factor
that’s driving that, it is the moral distress
1:38:21.340,1:38:26.110
in the situations like Mahée and Michelle
described here.
1:38:26.110,1:38:30.750
And so I think when we think about the peril
that our healthcare system is currently in
1:38:30.750,1:38:37.010
due to healthcare shortages due to rapid staff
departures and so on, we really do need to
1:38:37.010,1:38:42.050
target, to know about these experiences with
the moral distress to address the organizational
1:38:42.050,1:38:47.091
and systemic factors that underlie some of
this, and to provide the individual level
1:38:47.091,1:38:50.659
supports to healthcare workers and all healthcare
workers.
1:38:50.659,1:38:55.909
Be that food services workers, occupational
therapists, nurses, physicians, everyone in
1:38:55.909,1:38:59.340
the system who’s providing this service.
1:38:59.340,1:39:04.830
And the simple value of saying thank you,
I think cannot be underestimated.
1:39:04.830,1:39:09.969
I have been in basements of hospitals saying
thank you, and to see the look on people’s
1:39:09.969,1:39:17.830
faces when they hear, thank you for your service,
because this is service and your sacrifice.
1:39:17.830,1:39:21.630
And to say thank you, those simple words are
very powerful.
1:39:21.630,1:39:24.250
And I think the more we say it, the better.
1:39:24.250,1:39:27.010
So we want to say it again publicly here today.
1:39:27.010,1:39:34.380
When we talk about the neuroscience of trauma,
we certainly know that there’s a saying in
1:39:34.380,1:39:37.610
trauma that the body keeps the score.
1:39:37.610,1:39:42.260
And so among people who have experienced trauma,
for example, we see higher rates of heart
1:39:42.260,1:39:48.380
disease, obesity, diabetes, and other forms
of cardiovascular risk factors.
1:39:48.380,1:39:53.659
We also see changes in brain functioning and
brain structure.
1:39:53.659,1:39:58.469
And so we can see pat differences in the patterns
of the way that the brain works together in
1:39:58.469,1:39:59.469
concert.
1:39:59.469,1:40:03.699
And we can also see what’s called essentially
a loss of some of the tissue in the brain
1:40:03.699,1:40:08.280
with repetitive stress or even a single trauma
in some cases.
1:40:08.280,1:40:13.570
And so what we do with all the work that we
do is focused on helping to to help with some
1:40:13.570,1:40:17.610
of the impacts of those changes in the body
and in the brain.
1:40:17.610,1:40:23.659
With moral injury, in work that we’ve done
led by Ruth Lanius at the University of Western
1:40:23.659,1:40:27.389
Ontario, and with some graduate students that
we co-supervised and postdoctoral fellows,
1:40:27.389,1:40:34.389
Chantal Lloyd and Braden Tripo, we actually
had military members and public safety personnel
1:40:34.389,1:40:40.389
who had PTSD recall events that were associated
with moral injury for them.
1:40:40.389,1:40:45.460
So that could be, for example, being in the
combat theatre and seeing a baby going down
1:40:45.460,1:40:47.449
the river and being powerless to intervene.
1:40:47.449,1:40:50.070
That’s a description, that’s an apt description.
1:40:50.070,1:40:56.860
Or being a first responder who is not able
to go into a lake to save the person because
1:40:56.860,1:40:58.429
the rules of engagements say that they can’t.
1:40:58.429,1:41:03.070
And people talk about these moral injuries
and the consequences for their lives, just
1:41:03.070,1:41:06.610
like we hear here with healthcare workers.
1:41:06.610,1:41:12.739
And what we found is that when these public
service personnel and military members recalled
1:41:12.739,1:41:19.890
these events, we saw areas of the brain involved
in disgust light up.
1:41:19.890,1:41:20.890
They were active.
1:41:20.890,1:41:25.719
So that feeling in your stomach, like you’ve
been punched in the gut, that [part of] the
1:41:25.719,1:41:30.449
brain which is called the insula, and that
region was very, very active when these memories
1:41:30.449,1:41:32.750
were recalled.
1:41:32.750,1:41:37.570
We also saw that areas of the brain, so one
is the dorsal, it’s called the dorsal anterior
1:41:37.570,1:41:42.110
cingulate, [which is] sort of the middle of
the brain, that’s associated with shame and
1:41:42.110,1:41:43.280
guilt.
1:41:43.280,1:41:46.770
And that brain region, again, was very, very
active.
1:41:46.770,1:41:50.010
And the brain was trying to compensate for
this.
1:41:50.010,1:41:55.010
So the frontal part of the brain, which really
helps to regulate our emotions, it was trying
1:41:55.010,1:42:01.989
to dampen down those feelings of disgust,
the shame and the guilt, the feeling of moral
1:42:01.989,1:42:02.989
judgment.
1:42:02.989,1:42:06.350
The brain was working overtime to try to dampen
that down in a protective way.
1:42:06.350,1:42:14.119
And so what I would say these stories tell
us is they tell us the impact of trauma and
1:42:14.119,1:42:17.239
situations like moral injury on the brain.
1:42:17.239,1:42:22.909
This is an injury like all other injuries,
and there’s so much shame and guilt that surveils
1:42:22.909,1:42:23.909
mental illness.
1:42:23.909,1:42:30.720
But here we see the changes to the brain that
occur and we can show it in a picture.
1:42:30.720,1:42:31.720
This is what’s happening.
1:42:31.720,1:42:36.489
So I think that helps to again, explain the
experience and what happens in the brain makes
1:42:36.489,1:42:40.780
complete sense in terms of people feel like
they’ve had a punch in the gut.
1:42:40.780,1:42:43.530
And this lingers after the incident itself.
1:42:43.530,1:42:48.530
These are scans that could be taken four,
five, 10, 15 years later, and we’re still
1:42:48.530,1:42:54.739
seeing that punch to the gut in the brain.
1:42:54.739,1:43:03.190
What I love about neuroscience and the work
that you do, Margaret, is that when you see
1:43:03.190,1:43:10.219
that injury and the evidence of it, I hope
that it does take the onus off of individuals
1:43:10.219,1:43:12.239
who are thinking, why can’t I cope?
1:43:12.239,1:43:13.239
Yeah.
1:43:13.239,1:43:14.690
In fact, you are wired in a way.
1:43:14.690,1:43:21.320
We are all wired in ways to react to these
situations and it’s partially why your work
1:43:21.320,1:43:24.500
is so important.
1:43:24.500,1:43:30.050
In the few minutes we have left, I would like
to ask this whole panel about what you would
1:43:30.050,1:43:36.869
like to see workplaces do in order to lessen
the impact of moral distress on healthcare
1:43:36.869,1:43:37.869
workers.
1:43:37.869,1:43:41.850
If we have heard from Michelle that moral
distress is a part of the job for nurses right
1:43:41.850,1:43:47.739
now, what can workplaces do to lessen the
impact?
1:43:47.739,1:43:53.820
And I would also like to ask about what you
are seeing in terms of hope for how workplaces
1:43:53.820,1:43:54.840
are changing.
1:43:54.840,1:43:59.570
So we’ll just start, we’re going to cram a
lot into the last five minutes, okay everyone?
1:43:59.570,1:44:03.630
So I would just like to start with what you
would like to see workplaces doing.
1:44:03.630,1:44:05.780
Maybe Michelle, would you like to begin?
1:44:05.780,1:44:06.780
Sure.
1:44:06.780,1:44:12.989
Well, I do want to say that I think it’s encouraging
that workplaces are having this discussion
1:44:12.989,1:44:14.830
more openly.
1:44:14.830,1:44:19.020
So we would see, for example, in internal
newsletters that would come out, that they
1:44:19.020,1:44:24.920
would be advertising the mental health support
line for staff telling people what sort of
1:44:24.920,1:44:25.920
E.F.A.P.
1:44:25.920,1:44:30.989
resources were available for mental health
supports and including kind of mental wellness
1:44:30.989,1:44:31.989
tips.
1:44:31.989,1:44:37.110
Now that’s where it sometimes kind of fell
flat for people that I spoke with in the interviews.
1:44:37.110,1:44:42.810
And that’s where I think we could maybe do
a better job of increasing supports for people,
1:44:42.810,1:44:48.870
is engaging the frontline healthcare workers
and determining what types of mental health
1:44:48.870,1:44:51.650
supports are going to be most meaningful for
them.
1:44:51.650,1:44:57.469
So I would have people telling me that it’s
all very well and good to provide tips on
1:44:57.469,1:45:01.929
healthy sleep hygiene, but if they’re working
so many hours and then have family to take
1:45:01.929,1:45:07.610
care of that they don’t have the number of
hours in a day to be able to sleep like that,
1:45:07.610,1:45:11.619
then they’re not able to implement those types
of suggestions.
1:45:11.619,1:45:17.600
So really engaging the frontline healthcare
workers in helping to come up with the solutions
1:45:17.600,1:45:24.599
for what is going to support them best in
the workplace.
1:45:24.599,1:45:27.590
Mahée, would you like to add to that?
1:45:27.590,1:45:28.590
Yes.
1:45:28.590,1:45:29.590
Thank you.
1:45:29.590,1:45:30.590
Thank you, Michelle.
1:45:30.590,1:45:32.080
Thank you so much.
1:45:32.080,1:45:39.050
As a result of our research project, we formulated
recommendations and I’m going to place them
1:45:39.050,1:45:45.100
on the chat because I know that we are tight
on schedule, so I’m not sure that everybody
1:45:45.100,1:45:51.989
could see them, but maybe you can oppose them.
1:45:51.989,1:45:59.880
So, our recommendations are not one size fits
all recipe, but they aim to heal the working
1:45:59.880,1:46:00.880
environment.
1:46:00.880,1:46:03.800
So we are not into coping mechanism.
1:46:03.800,1:46:10.700
We really want to focus on the working environment
and on building a climate of kindness and
1:46:10.700,1:46:12.810
of psychosocial safety.
1:46:12.810,1:46:19.290
They are grouped into different categories,
and I’m going to just give you a few examples
1:46:19.290,1:46:21.840
really quickly.
1:46:21.840,1:46:23.210
First category is training.
1:46:23.210,1:46:31.050
So we really think it’s important to train
the leaders to detect the first signs of the
1:46:31.050,1:46:39.489
stress or of moral challenges in their employees
and to actively listen and support.
1:46:39.489,1:46:41.250
Second key is communicating.
1:46:41.250,1:46:50.170
So opening the gate of open, frequent empathetic
and leader-led team discussions to build awareness
1:46:50.170,1:46:57.120
and prepare for the situations that might
or that will come up.
1:46:57.120,1:47:04.100
Like Michelle says, having all levels of worker
participating in the intervention efforts
1:47:04.100,1:47:11.790
is crucial, and I’m going to end with prioritizing,
prioritizing mental health.
1:47:11.790,1:47:17.830
There are not a lot of resources in the healthcare,
but we cannot keep on pushing back.
1:47:17.830,1:47:21.199
This is a priority among the other priorities.
1:47:21.199,1:47:26.100
So that’s it for me for now.
1:47:26.100,1:47:27.510
Thank you.
1:47:27.510,1:47:29.219
Mahée, thank you so much.
1:47:29.219,1:47:34.300
I think you said that you had dropped the
link in the chat, but I don’t see it.
1:47:34.300,1:47:40.469
So maybe if you want to try that again in
the last few minutes or as well, I’m hoping
1:47:40.469,1:47:48.150
that Sangita can drop the link to the Healthcare
Salute website and socials and so afterwards,
1:47:48.150,1:47:52.940
I hope that everyone here can follow up for
further connection there.
1:47:52.940,1:48:00.260
Margaret, can I end with you in, in terms
of where you see hope, for how workplaces
1:48:00.260,1:48:03.980
are changing and incorporating these discussions
in the workplace?
1:48:03.980,1:48:04.980
Sure.
1:48:04.980,1:48:05.980
Thank you.
1:48:05.980,1:48:09.560
And so we asked healthcare records in the
interview, what is it that you need?
1:48:09.560,1:48:12.560
What would help you?
1:48:12.560,1:48:17.000
And many of these healthcare workers said
we want people to know our stories.
1:48:17.000,1:48:21.270
We want people to hear, we don’t want to have
to keep retelling them.
1:48:21.270,1:48:25.360
And when we go for mental health supports,
for example, that the person at the end of
1:48:25.360,1:48:28.250
the line isn’t crying when they hear our story.
1:48:28.250,1:48:32.110
And that often happens for public safety personnel
and military members.
1:48:32.110,1:48:38.850
They tell their stories to a mental health
professional and they end up comforting the
1:48:38.850,1:48:39.850
mental health professional.
1:48:39.850,1:48:40.850
And that’s difficult, right?
1:48:40.850,1:48:44.659
So we’ve been really fortunate to have funding
from the Public Health Agency of Canada, a
1:48:44.659,1:48:49.530
donation from Homewood Health, Centre of Excellence
on PTSD, and the Canadian Institutes of Health
1:48:49.530,1:48:53.560
Research, which is really hopeful, to see
all these agencies supporting this to develop
1:48:53.560,1:48:58.780
cultural competency or cultural sensitivity
around the experiences of healthcare workers.
1:48:58.780,1:49:05.210
And so, the courage we saw here today of healthcare
workers who told their stories and continuing
1:49:05.210,1:49:11.710
work to really get that knowledge out to the
public, to leaders, to policy makers, and
1:49:11.710,1:49:17.170
to others, we really have the opportunity
to provide supports that are culturally competent
1:49:17.170,1:49:21.550
and what people need and what they’re asking
for, and so that they don’t have to retell
1:49:21.550,1:49:24.370
their stories over and over again.
1:49:24.370,1:49:29.850
Well, thank you so much Margaret, and thank
you Mahée and Michelle.
1:49:29.850,1:49:37.820
And you know, I can see in the chat that there’s
a lot of reaction to the research and the
1:49:37.820,1:49:44.550
information that you’ve shared, and I also
just want to thank every participant who has
1:49:44.550,1:49:50.210
presented or spoken today, and especially
to the hundreds of people who showed up from
1:49:50.210,1:49:55.360
across the country to come and listen and
learn and to participate in the chat as well.
1:49:55.360,1:50:00.210
So Mahée, I think you said this is a priority
among priorities.
1:50:00.210,1:50:05.599
I couldn’t agree more, and I hope that everybody
here has gotten something out of the symposium
1:50:05.599,1:50:08.170
and that you can stay connected as well.
1:50:08.170,1:50:15.260
So there was a wellness slide earlier with
some mental health resources.
1:50:15.260,1:50:18.210
I hope that that can be shared again here.
1:50:18.210,1:50:23.850
And I just want to wish everybody a good day
and thank you so much for taking part.
1:50:23.850,1:50:24.850
Goodbye.
1:50:24.850,1:50:30.860
And thank you to all of you for your service.
1:50:30.860,1:50:31.860
We salute you.
Panelists

Dr. Margaret McKinnon, Homewood Chair in Mental Health and Trauma; Professor, McMaster University
Dr. Margaret McKinnon is Full Professor and Associate Chair, Research in the Department of Psychiatry and Behavioural Neurosciences at McMaster University, where she holds the Homewood Chair in Mental Health and Trauma. She is also the Research Lead for Mental Health and Addictions at St. Joseph’s Healthcare Hamilton and a Senior Scientist at Homewood Research Institute.
Work in Margaret’s unit focuses on identifying the neural and behavioural correlates of PTSD and trauma-related illnesses and on translating this knowledge to the development and testing of novel treatment interventions aimed at reducing the cognitive and affective sequelae of these conditions.
A licensed clinical psychologist and clinical neuropsychologist, Margaret has a special interest in military, veteran, and public safety populations (including healthcare providers), and has worked with these groups clinically and in her research program. She has published or in press nearly 150 scientific works.
Under Margaret’s leadership, the Trauma & Recovery Research Unit is supported by federal and provincial funding from the Public Health Agency of Canada, Canadian Institutes of Health Research, the Canadian Institute for Military and Veterans Health Research, Veterans Affairs Canada, Defence Canada, the PTSD Centre of Excellence, MITACS, and the Workers Safety Insurance Board of Ontario; by a generous donation to Homewood Research Institute from Homewood Health Inc.; and by generous gifts from private foundations including True Patriot Love, the Cowan Foundation, the Military Casualty Support Foundation, the FDC Foundation, and the AllOne Foundation.
Margaret is a frequent commentator in the media on matters related to PTSD, moral injury, and the impact of trauma on special populations.

Dr. Mahée Gilbert-Ouimet, Associate Professor, Université du Québec à Rimouski
Dr. Mahée Gilbert-Ouimet is associate professor in Population Health at the Université du Québec à Rimouski. She also holds the Canada Research Chair in Sex and Gender in Occupational Health. Dr. Gilbert-Ouimet received her PhD in epidemiology from Laval University. She also performed a first postdoctoral fellowship in epidemiology at the Institute for Work & Health and a second postdoctoral fellowship in health economics at the Université du Québec à Montréal.
Dr. Gilbert-Ouimet research mainly focuses on the adverse effects of psychosocial stressors at work on the incidence of chronic health problems, and on how to conduct intervention studies aimed at reducing these stressors. Dr. Gilbert-Ouimet has published 45 peer-reviewed articles and realized over a hundred knowledge transfer activities. In the context of the COVID-19 pandemic, she recently issued preliminary guidelines aiming to prevent and manage moral injuries in Canadian frontline healthcare workers. She also authored a Guide of organizational practices favourable to health that is now distributed by the Quebec Ministry of Health and Social Services to all health establishments of the province of Quebec. Dr. Gilbert-Ouimet is also actively involved in developing methods and recommendations aiming to improve sex and gender considerations in health research.

Dr. Michelle McCarron, Research Scientist, Saskatchewan Health Authority
Dr. Michelle McCarron is a Research Scientist with the Saskatchewan Health Authority (SHA). She is also an Adjunct Professor in the Faculty of Graduate Studies and Research at the University of Regina, where she is a Sessional Lecturer with the Department of Psychology. Dr. McCarron is a member of the Saskatchewan Centre for Patient-Oriented Research (SCPOR) Affiliated Researcher Alliance and the Canadian Institute for Public Safety Research and Treatment (CIPSRT) Academic, Researcher, and Clinician (ARC) Network.
Michelle holds a Ph.D. in Experimental and Applied Psychology from the University of Regina. From 2012-2017, she was the Chair of the Research Ethics Board (REB) for the Regina Qu’Appelle Health Region and now serves as the Vice Chair of the SHA REB. Her primary areas of research interest include frontline healthcare worker and Public Safety Personnel (PSP) mental health, evidence-informed decision-making within healthcare and PSP organizations, and research and professional ethics.
Dr. McCarron was the Principal Applicant on a study funded by the Department of National Defence Innovation for Defence Excellence and Security (IDEaS) program, titled “Operationalizing the Concept of Moral Injury within Canadian Frontline Healthcare Workers” and is the Nominated Principal Applicant on a CIHR-funded Mental Wellness in PSP project developing and pilot testing an online “Research 101” course promoting scientific literacy among PSP leadership to support evidence-informed decision-making in the provision of mental health care for frontline PSP.
Healthcare providers

Krissha Fortuna, RPN
Krissha Fortuna is a registered practical nurse who works in long-term care in Ontario.

Michelle Johnson, RN
Michelle Johnson is a registered nurse who works in Ontario.

Dr. Jennifer Kwan, Family Doctor
Dr. Jennifer Kwan tweets from @jkwan_md. Throughout the pandemic’s first many waves, she posted important, accessible data about #COVID19Ontario transmission to her Twitter feed. Dr. Kwan is a cofounder of the Masks4Canada volunteer group and the Doctors for Justice in Long-Term Care (Docs4LTCJustice) campaign.
She is a family doctor who practices in Ontario.
Presenters

Dr. Andrea Brown, Research Associate, Trauma & Recovery Research Unit, McMaster University
Dr. Andrea Brown obtained her PhD in Applied Social Psychology from the University of Guelph. In addition to her work in the Trauma and Recovery Research Unit, Dr. Brown has conducted applied research and program evaluation for not-for-profit organizations, regional government, the Department of National Defence, academe, and industry.
Since 2015, Dr. Brown’s focus has been on mental health and addictions research and evaluation, with a specialty on military sexual trauma (MST) and post-traumatic stress disorder. She is also the Co-Director of the MiNDS Network for MST and the Director of Knowledge Exchange for the Canadian MST Community of Practice.
In addition to this, Dr. Brown is currently completing a Masters in Psychotherapy at McMaster University.
Yuanxin Xue, Research Assistant, McMaster University
Yuanxin Xue is a medical student at the University of Toronto. He completed his Bachelor of Health Sciences and MSc in Global Health at McMaster University. Yuanxin’s current research focuses on various facets of mental health, perioperative medicine, as well as the intersections between these fields. He currently works as a Research Assistant at the Trauma & Recovery Research Unit.
Moderator

Hannah Sung, Co-founder, Media Girlfriends
Hannah Sung is a co-founder of Media Girlfriends. Her previous work includes producing award-winning podcasts for The Globe and Mail and the Globe Content Studio, including Colour Code, a podcast about race in Canada, and Stress Test, a podcast about personal finance in the pandemic. She executive produced award-winning podcasts at TVO and The Walrus Lab on social issues, politics, and current affairs. In 2020, she was the Asper Fellow at the University of Western Ontario’s Faculty of Information and Media Studies, where she led a post-graduate journalism class in narrative podcasting.
Hannah began her career in music television at MuchMusic, where she was the host of shows including MuchNews and the live red carpet at the MuchMusic Video Awards.
With gratitude to McMaster University Faculty of Health Sciences: Continuing Professional Development for broadcasting this event’s video feed.
